The human nervous system is an intricate thing, with nerve signals twisting and turning through structures called columns, roots, trunks, and cords on their way from the brain to the extremities and back again.
As complex as this labyrinth is, in most people its twists and turns are nearly identical. This allows an electromyographer to know what nerves innervate each part of the body and to reliably find and test those nerves during an EMG/NCS study.
In rare cases, however, a person’s nerve fibers may choose to take the “scenic route,” and travel along a different course to reach their destination. When this happens, it is called an anastomosis, and it can change the way an EMG/NCS study looks.
One tricky anastomosis is called the “ulnar hand.” In this article we will explore how this anastomosis works and how it affects EMG/NCS results in patients with nerve pathologies.
Anatomy of an Anastomosis
Ordinarily, the palm of the hand is innervated by two nerves—median and ulnar—which carry sensory nerve signals from the skin and motor signals to the muscles.
The median nerve is responsible for the muscles of the thumb and sensation for the first three-and-a-half fingers. The rest of the hand is covered by the ulnar nerve.

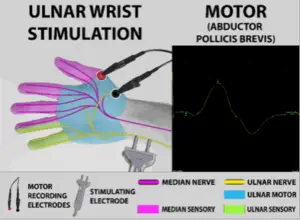
When a nerve conduction study is performed, you can expect that stimulating the median and ulnar nerves should result in healthy responses from their respective domains.
Case 1: Ulnar Hand Without Nerve Damage
In an “ulnar hand” anastomosis (the most pronounced form of the Riche-Cannieu anastomosis), however, the median nerve is still responsible for finger sensation, but the ulnar nerve innervates all or almost all the muscles of the hand.

Here is what it looked like in a 38-year-old woman without nerve damage.
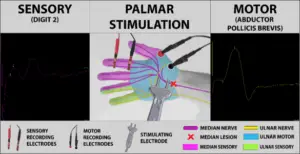
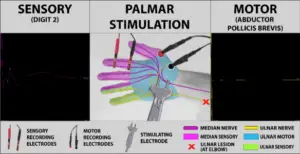
Electrical stimulation at the palm produced large, healthy-looking wave forms, which were recorded from the index finger and the abductor pollicis brevis muscle.
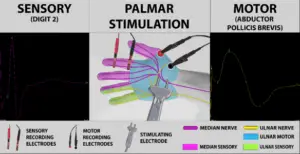
The sensory response from the finger was due to median nerve stimulation, but in this patient the excellent motor response came from stimulating the ulnar nerve, which runs very near the median nerve in the palm of the hand.
At the wrist, however, the median and ulnar nerves are farther apart, so stimulating at that point still produced good sensory responses, but the motor response disappeared.
Losing the median motor response at the wrist might have raised suspicion of severe carpal tunnel syndrome if the median sensory responses had not been so healthy.
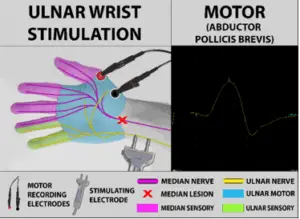
The selective absence of a median motor response at the wrist raises suspicion of an ulnar hand anastomosis. This is confirmed by stimulating the ulnar nerve at the wrist, which produces a large response from the thenar (thumb) muscles.
This case highlights the importance of considering both a patient’s motor and sensory nerve conduction findings, and the value of flexible thinking to avoid misdiagnosing a condition which, though not strictly “normal,” is not pathological.
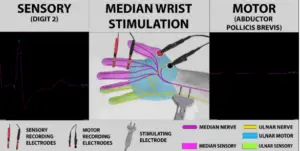
Case 2: Ulnar Hand with Carpal Tunnel Syndrome
Evaluating a patient with an ulnar hand anastomosis becomes more complicated when there actually is pathology at the carpal tunnel.
Consider these findings from a 68-year-old woman:
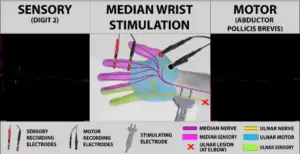
Just as seen in the first case, stimulating this patient’s palm produced a motor response at the thumb and a sensory response at the index finger, but this time the sensory response was much smaller and weaker.
Stimulating at the wrist, however, resulted in no motor or sensory response at all.
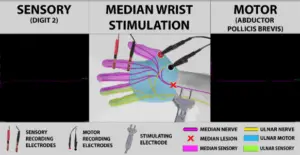
When interpreting these findings, the first impulse might be to assume that the patient had very severe carpal tunnel syndrome, such that no motor or sensory signals could travel past the compression at the wrist.
Such severe carpal tunnel syndrome typically results in loss of function in the affected muscles, but instead the patient had no symptoms or clinical signs of hand weakness. What’s more, needle EMG of the thenar muscles showed that they were firing normally
This led to stimulation of the ulnar nerve at the wrist. A healthy motor response was seen at the thumb, showing that the thenar eminence in this patient is innervated by the ulnar nerve.
In this case, the ulnar hand anastomosis is actually beneficial to the patient, because the carpal tunnel syndrome only caused sensory damage. Her strength was unaffected because all the muscles of his hand are innervated by the ulnar nerve, which circumvents the carpal tunnel.
Even so, the anastomosis makes it difficult to grade the severity of the carpal tunnel syndrome, since most grading scales rely heavily upon the median motor response at the wrist.
This patient demonstrates the importance of complementing nerve conduction studies with electromyography (EMG), and of considering electrophysiologic findings in the context of a thorough patient history and clinical examination. If these steps had not been taken, the anastomosis could have been overlooked, leading to an exaggerated appraisal of the carpal tunnel syndrome.
Case 3: Ulnar Hand with Cubital Tunnel Syndrome
Although the ulnar hand anastomosis mitigates the affects of median neuropathy, it makes an ulnar neuropathy far worse.
The third patient (a 65-year-old man), had a severe left ulnar neuropathy at the elbow (“cubital tunnel syndrome”). This was established by small, weak ulnar nerve motor and sensory signals, as well as slow conduction across the elbow and abnormal needle EMG findings in ulnar-innervated muscles.
Because he also had an ulnar hand anastomosis, however, his thenar muscles were also affected, with no response to stimulation at the palm.
There was also no motor response with stimulation at the wrist, but healthy median sensory responses were seen in both locations.
This case presented a greater diagnostic challenge than the two previous cases. Although ulnar nerve testing made ulnar neuropathy at the elbow clear, the loss of motor innervation to the thumb could also be explained by a superimposed cervical radiculopathy or brachial plexopathy. In order to rule out these possibilities, medial antebrachial cutaneous nerve testing and thorough EMG sampling in the C8/T1 myotome and the cervical paraspinals was required.
Conclusion
Partial innervation of thenar muscles by the ulnar nerve is known as a Riche-Cannieu anastomosis and is quite common. A recent meta-analysis found this “anomaly” in 55.5% of individuals, making it more the rule than the exception.
Most of the time, the ulnar contribution is minor and does not affect diagnostic testing significantly, but when the anastomosis is significant (the “ulnar hand”) it must be recognized in order to avoid inappropriate diagnosis and unnecessary surgery.
Thorough clinical and electrophysiologic testing work together to cut through the confusion that can surround cases like those discussed here, in order to provide clinicians and patients the most accurate and actionable information possible.