You’ve probably heard the expression, “measure twice, cut once.” Nowhere is that adage truer than in the field of medicine.
Electromyography and nerve conduction studies (EMG/NCS) are part of the measurement process which helps physicians provide the most accurate diagnosis and appropriate treatment for symptoms which can sometimes be rather vague.
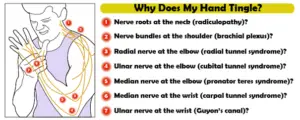
Take carpal tunnel syndrome (CTS), for example. This condition involves dysfunction of the median nerve at the wrist, and it usually manifests as numbness, tingling, and pain in the affected hand. But although carpal tunnel syndrome is the most common compression neuropathy, nerve damage in many other areas can cause similar symptoms.
I recently became curious about how often EMG/NCS confirms median neuropathy at the wrists in patients with carpal tunnel type symptoms, and how often other nerve disorders are identified. To examine this, I reviewed the reports of 338 patients referred for evaluation of carpal tunnel syndrome and cataloged their electrodiagnostic results.
In this post, I will list the most common electrodiagnostic findings I observed in patients referred for CTS evaluation, and will briefly review how these findings can impact patient care.
1. Median Neuropathy At The Wrist
In my patient population, EMG/NCS tests found median neuropathy at the wrist in 84% of the patients suspected of having CTS. This comes as no surprise of course. After all, if it looks like a duck and it quacks like a duck, chances are that it’s a duck.
For many of these patient’s however, the median nerve wasn’t the only culprit. 15% of patients had median neuropathy and nerve damage at one or more other sites. Furthermore, 1% of patients had other damaged nerves without median neuropathy, and 14% of studies found no nerve damage at all.
2. Cervical Radiculopathy
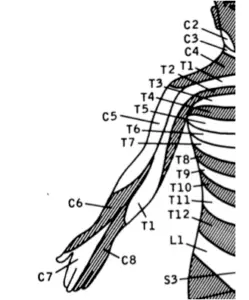
32 patients (9%) were found to have a cervical radiculopathic process, meaning that damage was occurring where nerve roots leave the spinal column.
The most common spinal level involved was C6. This makes sense because nerves from this level provide sensation to an area (called a dermatome) which includes the thumb. Because the thumb is also innervated by the median nerve, numbness or tingling coming from a C6 radiculopathy could easily be mistaken for carpal tunnel syndrome.
 ‘=
‘=
This can be a very important finding. If a patient has both cervical radiculopathy and median neuropathy at the wrist, then his or her physician can include both areas in the plan of care. Alternatively, if the neck is the only culprit then knowing this could save months of potential pain and confusion from unnecessary CTS treatments.
3. Ulnar Neuropathy At The Elbow
The median nerve provides sensation to the thumb, index, and middle fingers, and half of the ring finger, but nerve symptoms are notoriously non-specific, and patients with carpal tunnel symptoms often report numbness and tingling in the entire hand.
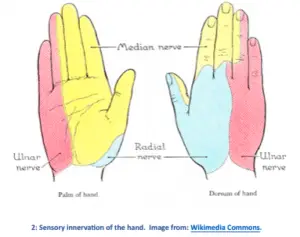
When this happens, it is important to know whether the ulnar neve (which goes to the other 1½ fingers) is involved. After carpal tunnel syndrome, ulnar neuropathy at the elbow (AKA “cubital tunnel syndrome”) is the second most common compression neuropathy.
Among the patients I studied, 9% turned out to have ulnar neuropathy. As with radiculopathy, this finding could have a significant impact of the course of care.
4. Radial Neuropathy
As seen in the image above, part of the hand’s sensation also comes from a third source—the radial nerve. Injury to this nerve is far less common than to the median and ulnar nerves, but when it does happen it can cause numbness in the thumb which may be confused with carpal tunnel syndrome.
Radial neuropathy was seen in 3 (1%) of the cases I reviewed. For two of these individuals, only the superficial sensory branch of the nerve was involved, meaning that the condition was unlikely to progress beyond numbness, tingling, and pain. In one case, however, the injury was more proximal, affecting the motor nerve fibers and causing severe atrophy and loss of function in the forearm and hand.
5. Polyneuropathy
Finally, 3% of patients with carpal tunnel-like symptoms had an underlying peripheral polyneuropathic process.
Polyneuropathies occur when genetic abnormalities, toxic chemicals, or underlying diseases cause the nerves to slow down and die. The hands and feet are typically affected first, causing pain, burning, and loss of sensation.
Not only can these symptoms mimic carpal tunnel syndrome, but the unhealthy nerves in a patient with neuropathy are prone to damage by other means, so that median and ulnar neuropathies are more likely to develop. It is important to know if a suspected CTS patient has a polyneuropathy because they will be less likely to have satisfactory outcomes from a carpal tunnel release surgery.
Summary
Most patients with carpal tunnel-type symptoms also tend to have carpal tunnel-type EMG/NCS findings, but at least 1 out of 6 patients will be glad that their doctor chose to “measure twice” before cutting.
Because nerve symptoms can be vague and more than a little deceptive, it is critical to know which nerves are involved in order to provide the best possible patient care.
On the other hand, it can be equally important to find out that nerves are fully functional, despite the numbness and tingling felt. You may have noticed that I haven’t gone into depth about the 14% of patients who had symptoms but no recordable nerve damage. This is an important topic, and it deserves an article all its own, so stay tuned for future posts!
In the meantime, if you are a physician feel free to reach out with any questions regarding how to use EMG/NCS more effectively in your clinic. If you’re already taking advantage of electrodiagnostic testing, you might consider checking out Darin White’s recent post on how to interpret electrodiagnostic reports so that you can get the most out of this extremely versatile diagnostic tool.


