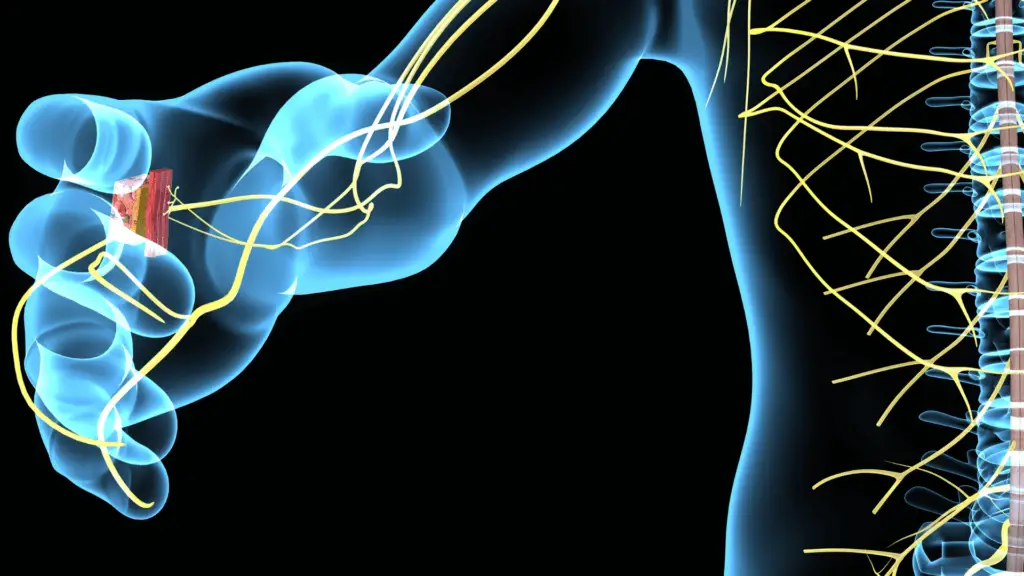
Evaluating the neuroanatomy of any patient is an important part of the clinical exam that is vital in making an accurate diagnosis. Just because a patient cannot raise their arm above their shoulder does not inherently mean their ailment is a musculoskeletal shoulder issue. There should be a list of possible diagnosis that need to be ruled out. Let us take for example the above mentioned shoulder patient. What are the possible diagnoses given this limited amount of information? They could have a labral tear, rotator cuff tear, axillary nerve lesion, brachial plexopathy, C5/C6 cervical radiculopathy, or frozen shoulder to name a few. The following 10 questions will help test your knowledge of neuroanatomy.
Which muscle is first innervated by the ulnar nerve?
A. First dorsal interosseous muscle of the hand
B. Abductor digiti minimi muscle
C. Flexor carpi ulnaris muscle
D. Flexor digitorum profundus to digits 4 and 5
Answer: C. Often the flexor carpi ulnaris muscle is spared with an ulnar nerve compromise at the cubital tunnel because the branch to the flexor carpi ulnaris splits off from the main trunk before the area of compression (Charles F Guardia, 2020). If the compromise is more proximal to the cubital tunnel, then the flexor carpi ulnaris will likely be involved.
Which nerve innervates the teres major muscle?
A. Suprascapular nerve
B. Dorsal scapular nerve
C. Upper subscapular nerve
D. Lower subscapular nerve
Answer: D. The lower subscapular nerve branches off of the posterior cord of the brachial plexus. There are three primary muscles that can be used to evaluate the posterior cord of the brachial plexus. The subscapularis, latissimus dorsi, and teres major. The subscapularis muscle can be challenging if not impossible to access with many patients. This is important because if both the latissimus dorsi and teres major muscles are both abnormal the problem is likely at the posterior cord. However, of these three muscles, only the latissimus dorsi muscle will be affected in an isolated thoracodorsal nerve compromise (Leis & Trapani, pg. 87).
Which muscle is typically spared with a radial nerve injury at the spiral groove?
A. Abductor pollicis longus muscle
B. Anconeus muscle
C. Supinator muscle
D. Brachioradialis muscle
Answer: B. The radial nerve sends a branch to the medial head of the triceps and anconeus muscles proximal to the spiral groove of the humerus (Leis & Trapani, pg. 41-43). Thus, even though the anconeus and supinator muscles are in close proximity to one another and they are both supplied by the radial nerve, the supinator will be abnormal while the anconeus will be normal.
What part of the brachial plexus does the nerve that innervates the pectoralis minor stem from?
A. Lateral cord
B. Posterior cord
C. Medial cord
D. Superior trunk
Answer: C. First of all, one must know that the pectoralis minor muscle is innervated by the medial pectoral nerve that stems from the medial cord (Leis & Trapani, pg. 94). Thus, in the case of a patient with an atrophied pectoralis major muscle understanding that the medial pectoral nerve stems from the medial cord while the lateral pectoral nerve (that innervates the pectoralis major muscle) stems from the lateral cord can help distinguish whether the patient suffers from an isolated lateral pectoral nerve compromise, a lateral cord compromise, or a brachial plexopathy (Leis & Trapani, pg. 1-5).
What is the pathway of innervation starting from the flexor pollicis longus muscle and working more proximal?
A. Anterior interosseous nerve, median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8, & T1.
B. Anterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7 & C8.
C. Median nerve, lateral and medial cords, middle and lower trunks, and roots C7 & C8.
D. Anterior interosseous nerve, median nerve, medial cord, lower trunk, and roots C8 & T1.
Answer: A. Understanding the pathway of a nerve can help distinguish all the possible places of compromise. For instance, a patient unable to flex the DIP of D1. If it were only an anterior interosseous nerve problem, then only the flexor pollicis brevis, flexor digitorum profundus (median portion) and pronator quadratus muscles should be affected. If it were a problem with the median nerve at the cubital fossa you would expect the abductor pollicis brevis to be added to the list of affected muscles. If the problem were still more proximal at the medial cord you would also see abnormalities in the first dorsal interosseous and flexor carpi ulnaris muscles in addition to all of the muscles listed previously.
What is the first muscle innervated by the femoral nerve?
A. Pectineus
B. Iliacus
C. Rectus femoris
D. Sartorius
Answer: B. Understanding that the iliacus muscle is the first muscle innervated by the femoral nerve will aide in diagnosing whether the femoral nerve compromise is proximal to the inguinal ligament or not. Since the branch of the femoral nerve to the iliacus muscle branches off proximal to the inguinal ligament. This muscle would be spared if the problem is at the inguinal ligament. If the problem is of the femoral nerve only, one would also expect to see abnormalities with the saphenous sensory nerve on the same side as well, since this is the continuing sensory branch from the femoral nerve (Leis & Trapani, pg. 165-174).
Which nerve is typically affected with tarsal tunnel syndrome?
A. Tibial nerve
B. Sural nerve
C. Saphenous nerve
D. Deep fibular nerve
Answer: A. Tarsal tunnel syndrome is caused by compression of the tibial nerve or its branches in the tarsal tunnel which is on the medial side of the ankle (Leis & Trapani, pg. 121). Patients normally complain of pain directly over the tarsal tunnel that radiates to the arch and plantar foot, as well as numbness/paresthesia of the plantar foot surface (Kiel, 2020). The sural, saphenous, and deep fibular nerves do not provide sensory nerve fibers to the plantar foot surface and would not be affected in tarsal tunnel syndrome.
Which nerve innervates the tensor fasciae latae muscle?
A. Femoral nerve
B. Obturator nerve
C. Superior gluteal nerve
D. Inferior gluteal nerve
Answer: C. The tensor fasciae latae muscle is innervated by the superior gluteal nerve which stems from the sacral plexus, and L4/L5/S1 nerve root levels. This is a good muscle to observe when suspicious of an L4 or L5 radiculopathy (Leis & Trapani, pg. 151).
If weakness and atrophy is present with the right hip adductor muscles, evaluation of which muscle would help distinguish a lumbar radiculopathic process versus an obturator nerve compromise?
A. Adductor longus
B. Vastus medialis
C. Medial head of the Gastrocnemius
D. Obturator externus
Answer: B. The adductor muscles of the leg are primarily innervated by the obturator nerve which stems from L2/L3/L4 nerve root levels. If the adductor muscles are atrophied, we expect to see abnormalities in the adductor longus muscle and while that would tell us about the obturator nerve it gives us no more information about the lumbar nerve root levels. The medial head of the gastrocnemius is innervated by the tibial nerve and stems from S1/S2 nerve root levels, which would not aide in distinguishing between an obturator nerve versus lumbar radiculopathic process. The obturator externus is also an obturator nerve innervated muscle, as well as inaccessible to direct observation. The vastus medialis is innervated by the femoral nerve which stems from L2/L3/L4 nerve root levels. Thus, if the vastus medialis is abnormal this will tell us that the problem is more proximal likely at the nerve root level, and if the muscle is normal the problem is likely an isolated obturator nerve compromise. (Leis & Trapani, pg. 175-181).
What is the pathway of innervation starting from the tibialis anterior muscle and working more proximal?
A. Superficial fibular nerve, common fibular nerve, fibular division of the sciatic nerve, sacral plexus, and roots L5 & S1.
B. Deep fibular nerve, common fibular nerve, fibular division of the sciatic nerve, lumbar plexus, and roots L4 & L5.
C. Superficial fibular nerve, common fibular nerve, fibular division of the sciatic nerve, sacral plexus, and roots L4 & L5.
D. Deep fibular nerve, common fibular nerve, fibular division of sciatic nerve, sacral plexus, and roots L4 & L5.
Answer: D. Understanding the pathway of a nerve can help distinguish all the possible places of compromise. For example, if a patient has left lower extremity foot drop where could the problem be located? If the tibialis anterior muscle is the only muscle atrophied with sparing of the extensor digitorum brevis muscle, there could be an isolated compromise to the branch of the deep fibular motor nerve to the tibialis anterior muscle. However, if the extensor digitorum brevis muscle is also affected the problem is likely more proximal. Thus, if EMG needle testing shows abnormalities in the fibularis longus muscle as well as the previous muscle mentioned, but not in the biceps femoris short head then the problem is likely at or near the fibular head (Leis & Trapani, pg. 135-145). If the problem is at or near the fibular head, then one would also expect the superficial fibular sensory nerve to be abnormal as well.
Medical diagnosis is tricky, and things are not always as they seem. Evaluating the neuroanatomy of any patient is a challenge and can be significantly aided with diagnostic tests such as Nerve Conduction Velocity studies (NCV) and Electromyography (EMG). If you or your patients are in need of expert evaluation look no further than EMG Solutions.

Kyle J. Martinos PT, DPT, ECS
- Charles F Guardia, I. (2020, November 04). Ulnar Neuropathy Clinical Presentation: History, Physical Examination, Ulnar neuropathy at elbow. Retrieved November 23, 2020, from https://emedicine.medscape.com/article/1141515-clinical
- Kiel, J. (2020, August 12). Tarsal Tunnel Syndrome. Retrieved November 30, 2020, from https://www.ncbi.nlm.nih.gov/books/NBK513273/
- Leis, A. A., & Trapani, V. C. (2000). Atlas of Electromyography. Oxford, NY: Oxford University Press.