Although carpal tunnel syndrome affecting the median nerve is designated as the most common entrapment mononeuropathy in the upper extremity, another player deserves honorable mention: the ulnar nerve in Guyon’s canal. EMG/NCV plays an important role in helping identify and localize a compromise of the ulnar nerve at the wrist.
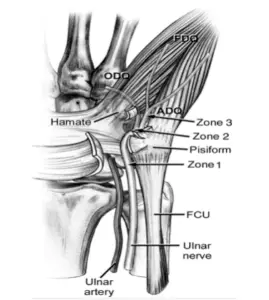
A brief anatomical review of Guyon’s canal highlights the structures surrounding the ulnar nerve through this infamous tunnel. The Floor: transverse carpal ligament and hypothenar muscles. The Roof: volar carpal ligament. Ulnar border: pisoform bone and pisohamate ligament and abductor digiti minimi muscle belly. Radial border: hook of hamate bone.
Patient’s typically present with a pattern of symptoms that may involve sensory deficits, motor deficits, or a combination of motor and sensory deficits. Most literature identifies 3 zones that are associated with the given clinical presentation and pattern of symptoms which is indicated by the location of the ulnar compromise within Guyon’s canal. A breakdown of these zones and corresponding deficits is clarified below.
(https://upload.orthobullets.com/topic/6022/images/zones.jpg)
Zone 1
Proximal to the bifurcation of the ulnar nerve into the deep branch and superficial branch. A compromise in this zone produces a clinical presentation of weakness in the dorsal and palmar interossei and hypothenar muscles in addition to decreased sensation in the distal palm, little finger and ulnar half of the ring finger. This is the most common area of compromise.
Zone 2
- Compromise proximal to division into deep branch and hypothenar branch. Clinical presentation of weakness in interossei and hypothenar muscles. No sensory deficits.
- Compromise distal to division into deep branch and hypothenar branch. Clinical presentation is weakness in all interossei muscles.
Zone 3
Compromise of only the superficial branch. Decreased sensation in the distal palm, little finger and ulnar half of the ring finger. No weakness present.
EMG/NCV is commonly utilized to evaluate ulnar nerve compromise when patients present with any of the above patterns of motor or sensory deficits. Typical complaints are sensory decreases with numbness in the ulnar distribution affecting the 4th and 5th fingers, possibly in conjunction with weakness of these digits.
Differential diagnosis includes ulnar neuropathy at the elbow or forearm, motor neuron disease, and C8-T1 cervical radiculopathy.
A few points in the clinical exam may help localize an ulnar compromise to the wrist level at Guyon’s canal. In evaluating the sensory distributions, should the patient have a deficit in the dorsal ulnar cutaneous nerve (DUC) distribution (dorsal ulnar hand), it is likely the lesion is more proximal since this nerve arises proximal to the wrist. Sensory deficits isolated the superficial sensory branch of the ulnar nerve help localize the compromise to wrist level. Likewise, should the patient have strength deficits in the flexor carpi ulnaris and flexor digitorum profundus, this points to a more proximal compromise since these muscles are innervated proximal to the wrist. Since these points are general guidelines, we must be aware of a few variables that my confound these findings: 1) Anomalous superficial radial innervation to the ulnar dorsum of the hand which produces an apparently “absent” DUC response and 2) Preferential fascicular involvement or sparing that occurs with an ulnar nerve lesion at the elbow—such as the Martin Gruber anastomosis which may present as a “conduction block” at the elbow.
Observation of muscle fasciculations, peculiar muscle atrophy patterns in the hand, neck pain with positive Spurling’s, and/or more global/proximal weakness may point to areas of involvement other than Guyon’s canal.
Electrodiagnostically it is beneficial to look at the following areas:
Nerve conduction studies should evaluate the Ulnar sensory to D5 superficial branch, Dorsal ulnar cutaneous (DUC), Ulnar motor nerve to abductor digiti minimi (ADM) and first dorsal interosseous (FDI) muscles due to preferential fascicular involvement to help detect Deep branch motor deficits.
EMG should evaluate ulnar distal and proximal innervated muscles to check for a more proximal compromise of the ulnar nerve and include muscles to exclude radiculopathy or other pathology. Key muscles include the abductor digiti minimi (ADM), first dorsal interosseous (FDI), Adductor pollicis (ADP), flexor digitorum profundus (FDP), and flexor carpi ulnaris (FCU) in addition to the cervical paraspinal muscles.
Once the compromise is isolated to the distal wrist in Guyon’s canal, ulnar inching technique recorded from the first dorsal interosseous muscle (FDI) can be employed to localize the compromise more accurately.
Compromise on the ulnar nerve in Guyon’s canal may be cause by ganglion cysts, sport activities such as bicycle riding with hands propped on handlebars, arterial aneurysms, lipomas, or occupation related with heavy use of the hands or postural positioning.
Fortunately we have an important tool with EMG/NCV to accurately evaluate Guyon’s canal ulnar nerve involvement and help such patients achieve pain relief and improved function.
At times, we sincerely hope it’s simply “All In The Wrist”!
Bibliography
Dumitru, D., Amato, A. and Zwarts, M., 2002. Electrodiagnostic medicine. Philadelphia: Hanley & Belfus.
Leis, A., 2013. Atlas of nerve conduction studies and electromyography. New York: Oxford University Press.
https://upload.orthobullets.com/topic/6022/images/zones.jpg



