Hereditary neuropathy with liability to pressure palsy (HNPP) or tomaculous neuropathy shares a molecular genetic relationship with Charcot Marie Tooth Disease type I (CMTI) in an autosomal dominant manner1. Most cases of CMT1A are caused by the duplication of 1.5mb in chromosome 17p11.2, while upwards of 85% of all HNPP cases are a result of the inverse of this mutation1. Mutations within the PMP-22 gene cab also cause HNPP1, 2, 3. The term “tomaculous” is derived from the focal globular thickening of the myelin sheath that resembles sausages, which are revealed during nerve biopsies1,3. The purpose of this case study is to provide electromyographers a clinical presentation of HNPP which will allow for a more accurate conclusion.
Patient Presentation
Patient is referred for electrodiagnostic testing for rule out of C5 nerve root compromise vs. suprascapular nerve injury secondary to a football injury. The patient is a 14 year old, right hand dominant, African American male who presents four weeks post a football injury that left his left shoulder numb with residual pain in the cervical spine. He reports that his numbness and tingling has resolved but still demonstrates residual weakness.
The clinical exam demonstrates discernible 3/5 weakness of the left deltoid, biceps, external shoulder rotators, and the ulnar hand intrinsics. MSRs were unable to be elicited throughout the left upper extremity. Special tests consisting of Tinel’s, Phalen’s, and Spurling’s cervical screen were all negative for the reproduction of the signs and symptoms.
NCV and EMG testing were obtained using a Cadwell Sierra Wave machine. Nerve conduction recording was performed using surface and finger clip electrodes. NCV testing was utilized on the bilateral median, ulnar, radial, and the left fibular motor nerves. Sensory testing was performed on the bilateral superficial radial, LABC, and the left superficial fibular, median, and ulnar nerves.
EMG studies were performed on the bilateral upper extremity muscles representing nerve root levels C5 through T1, the left lower extremity muscles representing nerve root levels L2 through S1, and the corresponding lumbar and cervical paraspinals.
Electrodiagnostic testing of the bilateral upper and left lower extremities revealed prolonged distal motor latencies of the bilateral median, ulnar, radial, and the left fibular nerve. Slow conduction velocities of the bilateral median nerves across the wrists, the bilateral ulnar nerves across the elbows, and the left fibular nerve across the fibular head were observed (TABLE 1).
Table 1:

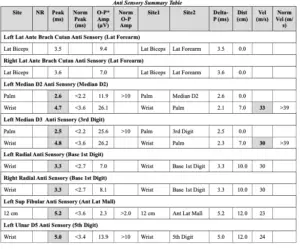
Sensory testing demonstrated prolonged distal sensory latencies of the bilateral superficial radial, and the left superficial fibular, median, and ulnar nerves. Slow conduction velocity of the left median sensory nerve across the wrist (TABLE 2).
Table 2:
F-wave studies, demonstrating long latency responses, were performed on the bilateral ulnar, median, and left fibular nerves. The left fibular, right median, and bilateral ulnar responses were found to be prolonged.
Needle electromyography demonstrate acute muscle membrane instability of the left deltoid, biceps, and first dorsal interosseous. Involvement of the left L4-L5 paraspinals was observed (TABLE 3).
The patient was referred to a pediatric neurologist for further delineation of findings.
Table 3:

Discussion
Manifestation of signs and symptoms is typically in the second to third decade of life, but some persons can remain asymptomatic1,2,3. Typical presentation is of a mononeuropathy secondary to minor trauma or some sort of compression such as wearing a backpack, resting on elbows, or crossing one’s legs3. Injuries are usually isolated to typical anatomical entrapment sites such as the wrists, elbows, and fibular head. Duration of numbness and weakness varies but typically fully resolves3. Electromyographers need to be cautious as electrophysiological presentation can be consistent with a progressive generalized or relapsing sensorimotor peripheral neuropathy such as CMT or chronic inflammatory demyelinating polyneuropathy, CIDP1.
When HNPP is a suspected diagnosis key nerves to include are those across in typical anatomical entrapment sites2. HNPP should be considered when a patient presents with a significant nerve compromise secondary to minor trauma.
References
- Dumitru D, Amato AA, Zwarts MJ. Electrodiagnostic Medicine, Second edition. Philadelphia: Hanley & Belfus; 2002.
- Bulusu S, McMillan HJ. A Report of Hereditary Neuropathy with Liability ot Pressure Palsy (HNPP) Presenting with Brachial Plexopahty: The Value of Complete Electrodiagnostic Testing. Am J Electroneurodiagnostic Technol. 2011;51:183-190.
- Flor-de-Lima F, Macedo L, Taipa R, Melo-Pires M, Rodrigues M. Hereditary Neuropathy with Liability to Pressure Palsy: A Recurrent and Bilateral Foot Drop Case Report. Case Reports in Pediatrics. 2014


