What is diabetes?
In 2018, an estimated 34.2 million Americans had diabetes, which was 10.5% of the population of the United States. Out of the 34.2 million estimated to have diabetes, 26.9 million had been diagnosed with the remaining estimated 7.3 million being undiagnosed. It was also reported that 88 million Americans aged 18 and older have prediabetes. Additionally, there were 1.5 million new cases of diabetes alone [6]. With such prevalence and increased incidence in the country, it is important to understand what diabetes is, the consequences to the individual, and how it can be prevented.
So, what is diabetes? Diabetes is a metabolic disease that causes hyperglycemia- also known as high blood sugar. The cause of the high blood sugar is caused by defects with either insulin secretion, insulin action, or a combination of both. Insulin helps to decrease blood sugar by inducing the uptake of glucose by the cells. There are 3 main types of diabetes: type 1, type 2, and gestational.
Type 1 diabetes is mainly diagnosed in younger individuals, usually after the age of 5. However, it can be diagnosed or seen in babies, toddlers, or even after the age of 30, but it is less common. Type 1 diabetes is caused by an autoimmune destruction of the β-cells in the pancreas that produce insulin, so the body is no longer able to produce insulin. Individuals with type 1 diabetes require an external source (like an insulin pump) of insulin to help with blood sugar regulation. Symptoms that may trigger the need to evaluate for type 1 diabetes include intense thirst, fruity smelling breath, acting drowsy, urinating excessively, and more.[1]
Type 2 diabetes is the most common type of diabetes. It is usually found in individuals who are 45 years old or more, have a family history of diabetes, and are overweight or obese [1]. The cause of type 2 diabetes comes from the cell’s resistance or decreased response to insulin, but it is often a combination of the body producing less insulin and the cells resistance or response to insulin. Symptoms for type 2 diabetes are the same as type 1.
Gestational diabetes is the type of diabetes that occurs only in pregnancy. The cause of gestational diabetes is sometimes associated with hormonal changes with pregnancy, but genes and weight may also play a role. The signs and symptoms are either not present or mild in severity- like being thirstier than usual or having to urinate more frequently.
How is diabetes classified/diagnosed?
If you or a family member are experiencing some of the signs and symptoms associated with diabetes, you can go to a doctor and have them order labs and other tests that will help to diagnose if you have diabetes, and what type you have.
There are multiple tests that can be performed to test if you are hyperglycemic (i.e., high blood sugar). They include the hemoglobin A1C (HbA1C), fasting plasma glucose (FPG), 2-h plasma glucose, and random plasma glucose (RPG). A diagnosis of diabetes would come with one of the following test results [1]:
- An HbA1C ≥6.5%- performed in laboratory using a method that is NGSP certified.
- Fasting Plasma Glucose (FPG) ≥126 mg/dl (7.0 mmol/l). Fasting is defined as no caloric intake for at least 8 hours.
- 2-hour plasma glucose ≥200 mg/dl (11.1 mmol/l) during an oral glucose tolerance test.
- In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dl (11.1 mmol/l).
For a diagnosis of type 1 diabetes, they will also perform a blood test to assess for certain autoantibodies that attack the β-cells in the pancreas. Since type 2 diabetes is not an autoimmune response, it would come back negative for the autoantibodies. A positive test for the autoantibodies would indicate having type 1 diabetes.
For gestational diabetes, the doctor will usually have a glucose challenge (or screen) performed. If your blood glucose from that test is >140 mg/dl, then the oral glucose tolerance test will be performed where blood will be drawn before the test and every hour for 3 hours after drinking the liquid glucose. If the blood sugar is high at 2 of any of the testing periods, that is a positive test for gestational diabetes.
Complications of diabetes
Having diabetes is more than just having problems with high blood sugar. It can lead to many other complications and medical conditions throughout the body. Long-term complications include kidney failure, loss of vision, nerve damage, cardiovascular damage, autonomic neuropathy, and they often have hypertension and cholesterol abnormalities.[1]
The nerve damage caused mainly consists of peripheral neuropathy. Neuropathy means there is a nerve compromise or dysfunction, and it is fairly prevalent in individuals with diabetes. Diabetic peripheral neuropathy affects at least 20% of type 1 diabetes patients by 20 years after onset. It is already affecting 10-15% of newly diagnosed type 2 diabetics and increases to 50% of type 2 diabetic patients 10 years after diagnosis.[2] Having diabetic neuropathy increases the risk for falls, increases pain, and decreases the individual’s quality of life. The cost of diabetic neuropathy and the complications associated with it are more than $10 billion in the United States annually.[3]
Diabetic Peripheral Neuropathy Symptoms
There are four main types of peripheral neuropathy that are diabetes related. These include distal symmetric polyneuropathy, autonomic neuropathies, focal neuropathies, and radiculopathies.[3]
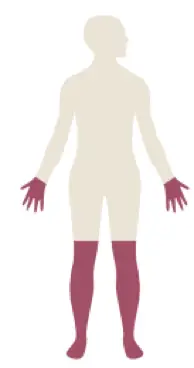
The most common form is call distal symmetric polyneuropathy. It commonly presents with numbness and tingling in the hands and lower legs- often called a “stocking glove distribution” as seen in the image to the right. With this condition, balancing can become more difficult because of the numbness of the feet, it can be harder to do fine motor tasks with the hands- like writing, holding change, and buttoning buttons- and burning symptoms may be felt in the feet and hands that are more noticeable when sitting still or laying down at night.
Autonomic neuropathies involve the function of the internal organs that are controlled by the autonomic nervous systems. Types of autonomic neuropathy include cardiac autonomic neuropathy, gastrointestinal dysmotility, diabetic cystopathy and impotence. Cardiac autonomic neuropathy is one of the more serious complications for diabetes in that it affects the nerves that innervate the heart and blood vessels leading to problems with heart rate control, dizziness with positional changes, heart attacks, intolerance to exercise, and more. Gastrointestinal dysmotility affects the organs that coordinate digestion which can lead to bloating, nausea, vomiting and even malnutrition. Diabetic cystopathy affects the bladder causing decreased bladder sensation, increased bladder capacity, and impaired bladder muscle contraction with urination. Finally, impotence is sexual dysfunction, usually associated with erectile dysfunction. [5]
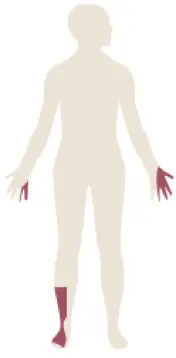
Focal neuropathies include conditions that affect a singular nerve, usually at common locations of compromise in the body. These compromises include conditions like carpal tunnel syndrome, cubital tunnel, fibular nerve compromise at the knee, and more. Carpal tunnel usually causes numbness to the thumb, index finger, middle finger, and part of the ring finger as well as weakness with gripping, fine motor tasks, and dropping things. Cubital tunnel syndrome is a problem with the ulnar nerve around the elbow and leads to numbness in the ring and pinky finger and can also lead to difficulty with fine motor tasks with the hands. The fibular nerve compromise at the knee can lead to numbness along the top of the foot and right side of the shin along with foot drop, where there is difficulty bringing the ankle up while walking and can lead to the foot getting caught on the ground or a step when walking. The location and symptoms of these three conditions can be seen in the image on the left.
The last peripheral neuroapthy that may occur from diabetes is a radiculopathy. A radiculopathy is a compromise of the nerves close to the spine after it comes off the spinal cord. It is often called a “pinched nerve” and is usually associated with pain in the low back or neck, numbness and tingling into the legs or arms, as well as weakness in the arm and leg muscles associated with the nerve root being pinched.
Causes of Nerve Damage for Distal Symmetric Polyneuropathy
There is a plethora of ways that diabetes leads to nerve damage. Research is still being performed to assess the cause, but the following are ways that diabetes causes nerve damage or dysfunction.[3]
- Diabetes affects circulation, especially the small blood vessels. Research has shown that dysfunction with the small blood vessels leads to peripheral nerve dysfunction.
- Prolonged high blood sugar leads to a slowing of the nerve with damage to Schwann cells.
- Diabetes affects the way the nerve cells process proteins, causing oxidative damage, and dysfunction of the mitochondria (which provides energy to the cells) that all ultimately lead to dysfunction of the peripheral nerves.
- The progressive diabetes leads to a dying back of the terminal ends of the nerves that connect to the skin or muscles.
In the case of distal symmetric polyneuropathy, the sensory nerves (nerves which supply sensation to the skin) are preferentially targeted, followed by autonomic nerves, and then to the motor nerves (nerves to the muscles). This is the reason why individuals experience numbness, tingling, burning, and other sensations before weakness with the muscles and other organ failure. Diabetic neuropathy also tends to affect the longest nerve fibers first, which is why an individual experiences a ‘stocking and glove’ pattern of numbness and tingling versus sensation abnormalities further up the legs and arms. As the diabetes progresses in severity, the longest motor nerves are then affected which is seen with less function in the small foot and hand muscles.
Risk Factors for Developing a Diabetic Neuropathy
The greatest and most common predictor for developing a diabetic neuropathy is related to two things: how long an individual has had diabetes and their HbA1C. Some other factors that are commonly associated with diabetic neuropathy include: obesity, increased triglyceride levels, hypertension, abdominal obesity, low HDL levels as well as some lifestyle factors that include smoking and alcohol abuse. [3]
Testing and Screening to Assess for Diabetic Neuropathy
Screening for diabetic neuropathy regularly is recommended. The American Diabetes Association recommends that screening for neuropathy should be performed for type 2 diabetes at the initial diagnosis and then yearly afterwards. For type 1 diabetics, it should be performed 5 years after diagnosis and then yearly. There are several tests that can be performed to assess for neuropathy including the following:[3]
- The 10 g monofilament test.
- Vibration testing with a 128Hz tuning fork.
- Assessing the deep tendon reflexes.
- Questionnaires (i.e., Michigan Neuropathy Screening Instrument)
Another way to test for diabetic neuropathy and its severity is to have a nerve conduction study (NCS) and electromyography (EMG) performed. It is a test of your nerve function- including the conduction speed and how the nerve fibers are functioning. According to some research, the nerve conduction speed is the most sensitive test to diagnose diabetic neuropathy.[6] Another benefit to having your nerves tested through NCS and EMG allows for the assessment of any focal neuropathies and radiculopathies as described above. A nerve test can be ordered by a physician.
Prevention of a Diabetic Polyneuropathy
As shown above, diabetic neuropathy can cause many problems and will affect the quality of life for the individuals who develop it. According to the current research, diabetic polyneuropathy cannot be cured, so prevention is needed. Research gives recommendations for prevention based on the type of diabetes an individual suffers from. For type 1 diabetics, there is a higher chance of prevention if they can keep intensive blood sugar control with an A1C under 6%. For individuals with type 2 diabetes, it is recommended to have an A1C of at least between 7.0 and 7.9% (or lower) as well as lifestyle modifications that include physical exercise, dietary control, and control of cardiovascular factors. Of the lifestyle changes suggested, moderate aerobic physical exercise is emerging as an important preventative measure for diabetic neuropathy in individuals with type 2 diabetes.
There are many resources available to the public to help teach about diabetes, how to prevent it, and how to manage it. Some of these resources can be found online through The American Diabetes Association and The National Institute of Diabetes and Digestive and Kidney Diseases. Primary care physicians should also be able to provide resources or provide direction to other local resources available.

Randall Hulet, PT, DPT
Board Eligible
Citations:
- American Diabetes Association (2010). Diagnosis and classification of diabetes mellitus. Diabetes care, 33 Suppl 1(Suppl 1), S62–S69. https://doi.org/10.2337/dc10-S062)
- Carvajal-Moreno, L., Coheña-Jiménez, M., García-Ventura, I., Pabón-Carrasco, M., & Pérez-Belloso, A. J. (2022). Prevention of Peripheral Distal Polyneuropathy in Patients with Diabetes: A Systematic Review. Journal of clinical medicine, 11(6), 1723. https://doi.org/10.3390/jcm11061723
- Feldman, E. L., Callaghan, B. C., Pop-Busui, R., Zochodne, D. W., Wright, D. E., Bennett, D. L., Bril, V., Russell, J. W., & Viswanathan, V. (2019). Diabetic neuropathy. Nature reviews. Disease primers, 5(1), 41. https://doi.org/10.1038/s41572-019-0092-1)
- Tehrani KHN. A Study of Nerve Conduction Velocity in Diabetic Patients and its Relationship with Tendon Reflexes (T-Reflex). (2018) Open Access Maced J Med Sci. 2018;6(6):1072-1076. Published 2018 Jun 17. doi:10.3889/oamjms.2018.262
- Vinik, A., Ziegler, D. (2007). Diabetic Cardiovascular Autonomic Neuropathy. Circulation 115:387–397. https://doi.org/10.1161/CIRCULATIONAHA.106.634949
- What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes. Accessed May 27, 2022.