EMG Solutions’ Physical Therapists, Austin Andrus, PT, DPT ECS, Kyle Martinos, PT, DPT, ECS, and Phil Hartley, PT, ECS presented on “Complex Nerve Injuries and Neuromuscular Disease in COVID-19 Survivors: A Case Series.” to a packed house. The room was filled to capacity and additional chairs had to be brought in! Attendees reported that “They did a great job!” and “Really good!” Attendees also posed many good and insightful questions both during and after the presentation. All-in-all it was a very informative presentation dealing with a current and relevant topic, providing insight into some of the complications of nerve injuries related to COVID-19 illness.
Some highlights from the presentation included Dr. Andrus presenting the case of a 23-year-old woman who developed sciatic and femoral nerve injuries in her left thigh while hospitalized with COVID-19. He discussed the deductive reasoning process that guided which tests he selected, and which ultimately led to an accurate diagnosis in this challenging case. He also commented on possible origins for the patient’s injury, including hospital positioning, use of medical devices on the leg, and thrombosis.
Dr. Andrus also presented the case of a 50-year-old man who recovered from a severe case of COVID-19 with generalized weakness in his extremities. He reported findings from two consecutive studies which helped to identify that the patient was most likely in recovery from COVID-associated AIDP. He discussed the way to differentiate AIDP from other forms of GBS, and from critical illness polyneuropathy/myopathy. While on the topic of critical illness polyneuropathy, he briefly addressed some post-COVID patients who might have been candidates for this diagnosis and showed evidence that illness-associated nerve injuries may occur even in individuals who do not require hospitalization. Finally, he commented on the AIDP patient in the larger COVID context, addressing whether a COVID diagnosis should cause more concern about GBS than other possible triggers.
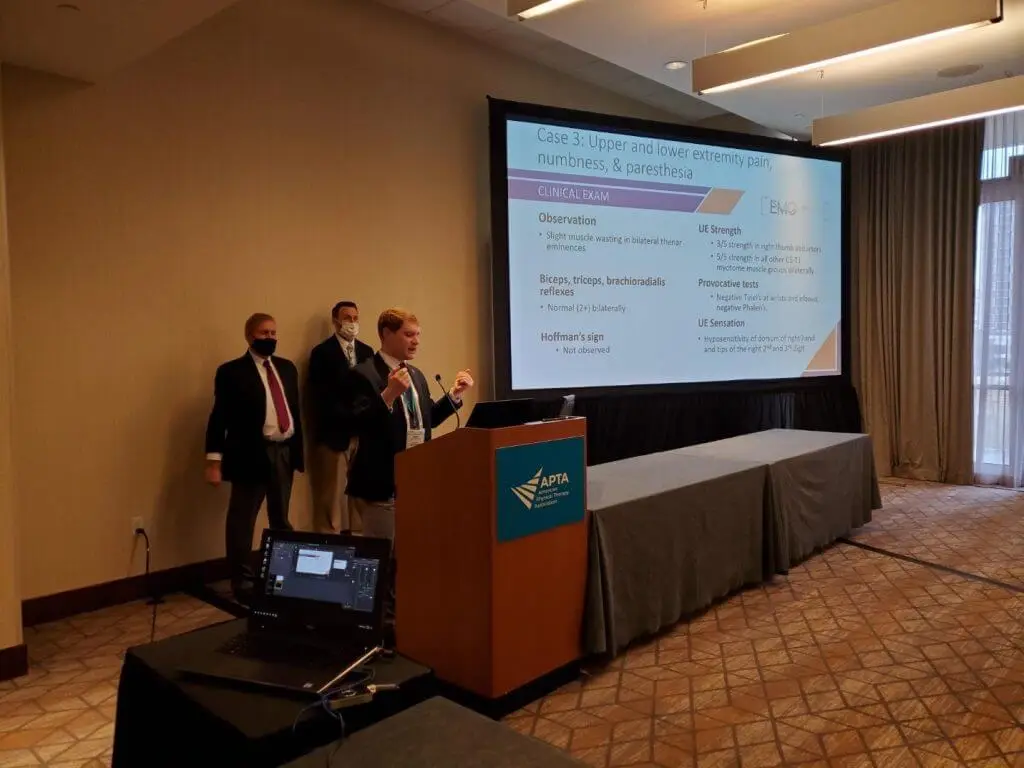
Dr. Martinos discussed how COVID-19 in a hospitalized patient contributed to their eventual brachial plexus compromise. He referenced in the literature how brachial plexus injuries, due to COVID-19, could come from several sources including a hypercoagulable state due to prone positioning and Parsonage-Turner Syndrome. However, prone positioning in and of itself seems to cause an increase in nerve related injuries, with brachial plexus compromises among those, especially in patients over 60 years old. With the rise in prone positioning that we are seeing with COVID-19 patients the more likely we are to see brachial plexopathies. Studies have reported that 73% of ICUs use prone positioning to treat COVID-19 patients. These patients have an average age of 60 years old and given the fact that 64% of brachial plexopathy patients were over 50 years old, according to Gutkowska et.al. in a 2018 literature review of 8700 patients, indicates that the likelihood of seeing a rise in plexus issues is a very real possibility. Dr. Martinos discussed possible mitigating factors and how we as physical therapists in an acute hospital setting might address these issues.
Dr. Hartley introduced the presentation with a brief outline of COVID-19 with the number of US hospitalizations and number of US deaths. He also discussed the number of worldwide cases followed by the number of global deaths and previewed the number of deaths as related to the number of hospitalizations. Dr. Hartley outlined the impact of COVID-19 on patients’ families, healthcare workers, as well as its affect on business and industry. He outlined COVID-19 related peripheral nerve injuries, neuromuscular injuries, critical illness polyneuropathies, and myopathies. He highlighted the impact of prone positioning especially with and without mechanical ventilation and the increased risk of peripheral nerve injury. Indications were given of studies done by other practitioners as compared to studies done by providers in our practice with a breakdown of COVID-19 related injuries and their prevalence by percentage of occurrence. He briefly discussed the role of frequent positioning changes for patients in the prone position and highlighted a few comorbidities in both general population and COVID-19 related patients. Dr. Hartley finished with the importance of electrodiagnostic testing and its role in helping improve our treatment of COVID-19 related injuries in patients by trying to identify conditions early in an effort to optimize patient treatments and outcomes.