If you have read many of my articles, you have probably noticed that I like to refer to electrophysiologic testing as “EMG/NCS.” Although this acronym is much shorter than the tests’ other names (like “electrophysiologic testing”) it is still a bit of a mouthful, and many people prefer to shorten it even further to simply “EMG,” or “NCS.”
Although there is nothing wrong with efficiency, because of these shortened names I have had some patients react with surprise when I tell them that there will be two parts to their test. Some say, “I was told I was getting a nerve conduction study [or EMG]—do I really need anything else?”
The short answer is…yes.
For the long answer, keep on reading.
In this article, I will explain how the two parts of an electrophysiologic test are distinct in their strengths and weaknesses and how they support each other in a symbiosis so complete that most insurance companies won’t even pay for one without the other.
Nerve Conduction Studies
Without diving into too much detail (click here if you would like more explanation), nerve conduction studies (NCS) involve stimulating nerves with small amounts of electricity and then recording signals carried by those nerves to determine the size and speed of their responses.
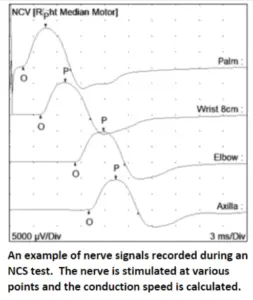
NCS is particularly helpful in identifying damage to the insulating myelin sheath of a nerve, which affects its conduction velocity. To a lesser degree it can also help in recognizing damage to the nerve fibers (called axons) themselves.
Some limitations to NCS include that nerves must be close to the surface of the skin in order to stimulate them, so some deeper nerve branches cannot be easily tested. Also, if myelin is not damaged, then NCS may not detect axon loss until it has become severe.
Electromyography
Electromyography (EMG), on the other hand, uses a small needle electrode to translate electrical activity in the muscles into waves on a screen, similar to an electrocardiogram (ECG). The results can reveal whether a muscle has lost nerve axons that should have innervated it, how long the problem has existed, and how the patient is progressing through stages of nerve healing.

EMG offers a very comprehensive understanding of axon loss, and because it uses a subcutaneous needle electrode, it can be performed on muscles deep below the skin. EMG is also one of the best methods for identifying diseases of muscle tissue.
EMG results are only abnormal when axons or muscle cells are affected, however; it offers no insight into the conduction velocity of a nerve, and its ability to discern the exact location of a nerve lesion is more limited than NCS.
It Takes Two to Tango
EMG and NCS are complementary tests—the limitations of one are the strengths of the other, and vice versa.
Most neuromuscular disorders can be diagnosed through a combination of EMG and NCS findings.
For example, let’s imagine that an EMG test finds signs of nerve axon loss in the flexor carpi ulnaris, first dorsal interosseous, and abductor pollicis brevis muscles. These muscles are innervated by motor nerve fibers which begin at the C8 and T1 nerve root levels in the neck, and which travel through the median and ulnar nerves.
So where is the pathology? Is it at the neck? Is it in the median and ulnar nerves?
The only way to know is to perform an NCS test. If NCS shows that the median and ulnar nerves are conducting normally, and if there is no damage to sensory nerve fibers, then it is clear that the problem stems from nerve roots in the neck.
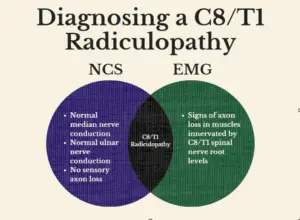
If the electromyographer only performed EMG tests then he or she would know there was a problem, but wouldn’t be able to localize it. On the other hand, if only NCS was performed then it is possible that the problem might have been missed altogether! Accurate diagnosis requires the unique contributions that both EMG and NCS bring to the table.
The same is true of almost every neuromuscular disorder. It is the combination of findings from the two tests that provide truly useful information.
Ruling in and Ruling Out
Another important reason to always complete both EMG and NCS tests during the same visit, is that it helps to screen for a greater number of disorders.
In a few cases, EMG or NCS findings alone may be clear enough to identify a disorder, but that doesn’t mean that the other test should be skipped. As I mentioned in another post, patients often have several overlapping neuromuscular conditions, and important things may be missed if a test is incomplete.
Let’s imagine that a patient has a C6 radiculopathy and moderate carpal tunnel syndrome. Both conditions can cause numbness in the thumb and index finger. The patient is referred for a cervical MRI and for electrophysiologic testing. The MRI shows foraminal stenosis at C6. If a lazy clinician saw C6 axon loss during his EMG and decided to skip the NCS, then the carpal tunnel syndrome would never be diagnosed!
Imagine this patient receiving a cervical surgery only to return to their physician in confusion because the numbness had not gone away.
This would never happen if a complete EMG and NCS test was performed.
A Dynamic Duo
Peanut butter and jelly, Batman and Robin, EMG and NCS: Some things are just made to go together.
But don’t just take my word for it! Consider some of these statements by national authorities:
“When NCSs are performed without needle EMG, the additional and complementary information provided by the needle EMG results…is not available. Without [this information], valuable data that may be essential in establishing an accurate diagnosis is missing. … It is important that NCSs and EMG examination be performed together and their results integrated into a unifying diagnostic impression.”
~American Association of Neuromuscular and Electrodiagnostic Medicine Position Statement
“Nerve conduction studies performed independent of needle electromyography (EMG) may only provide a portion of the information needed to diagnose muscle, nerve root, and most nerve disorders. When the nerve conduction study (NCS) is used on its own, without integrating needle EMG findings,” or when an individual relies solely on a review of NCS data, the results can be misleading, and important diagnoses may be missed.”
~Centers for Medicare and Medicaid Services (CMS) Billing and Coding Guidelines
A complete electrodiagnostic test (with all its parts), is a powerful, sensitive and specific tool for identifying a wide range of neuromuscular disorders. It can provide the information needed for a host of life-changing treatments.
If you are a healthcare provider who uses electrodiagnostic tests, I encourage you to remember to use the important information provided by both halves of the EMG/NCS reports you read. If you are a patient surprised to hear that you will be getting more testing than you expected, I hope you will now see this as a pleasant surprise, and proof that you are getting the best possible care!