There are many causes of shoulder pain because of the plethora of structures that are involved with passive and active stability and mobility of the glenohumeral joint, clavicle, scapula, and cervical spine. Of the many causes of pain, weakness, or dysfunction in the shoulder, one to consider is a suprascapular nerve compromise or neuropathy. In this blog post, we will go over the path and anatomy of the suprascapular nerve, what can cause problems or injury to it, how to examine or assess for it, and how it is diagnosed.
Path of the Suprascapular Nerve
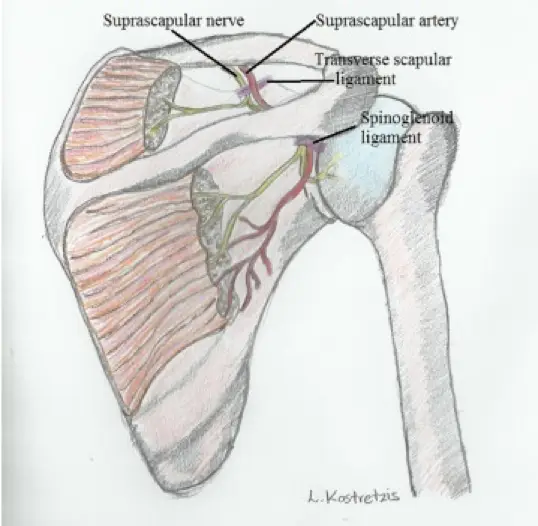
The suprascapular nerve predominantly provides motor nerve innervation to the supraspinatus and infraspinatus muscles. Research shows that it also provides sensory innervation for the coracohumeral ligament, the coracoclavicular ligament, the subacromial bursa and the posterior shoulder capsule.3
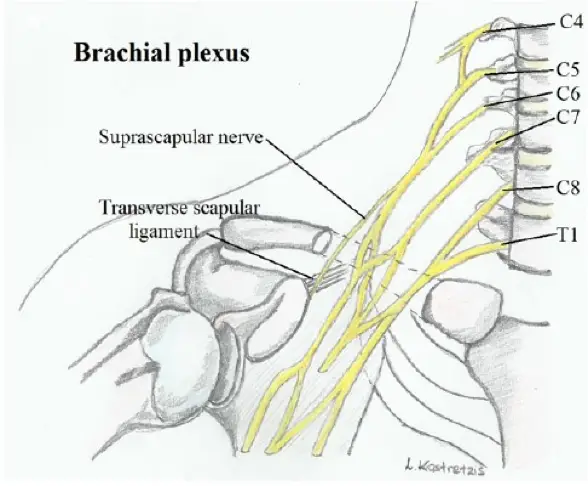
The suprascapular nerve comes off the upper trunk of the brachial plexus with originations from the C5 and C6 ventral rami, with occasional involvement from the C4. It proceeds laterally through the posterior cervical triangle, posterior to the clavicle, across the superior border of the scapula and into the suprascapular notch. As it crosses into the supraspinatus fossa it innervates the supraspinatus muscle and receives sensory branches. It then continues through the spinoglenoid notch, underneath the spinoglenoid ligament, and terminates with the innervation of the infraspinatus.1
Pathogenesis
There are multiple locations and causes of a suprascapular neuropathy. The main sites for the entrapment and compression of the suprascapular nerve include the following2:
- Suprascapular notch
- Spinoglenoid notch
- Superior transverse scapular ligament
Some causes of the nerve compression at these locations include, but are not limited to, the following1,2:
- Variations of the suprascapular notch.4
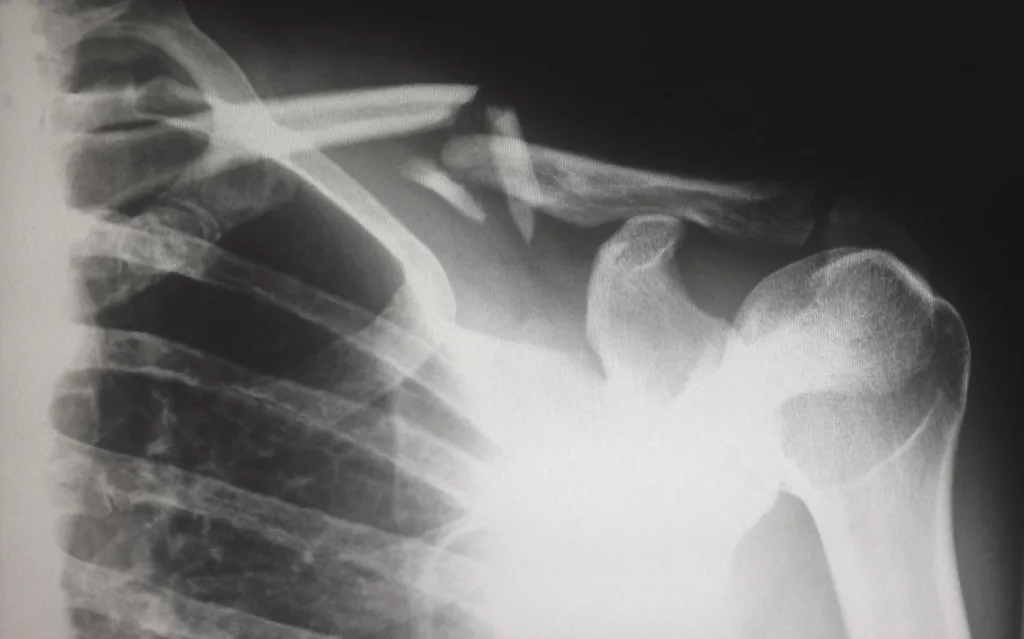
- Fractures of the scapula and clavicle and associated scar tissue
- Space occupying lesions6
- Enlarged spinoglenoid veins
- Lipomas
- Intraosseous ganglion cysts
- Supraglenoid or spinoglenoid cysts
- Paralabral cysts
- Retracted rotator cuff muscles from tears7
- Abnormal subscapularis muscle fibers covering the suprascapular notch5
- Ligament abnormalities
- Anterior coracoscapular ligament5
- Calcified suprascapular ligament 5
- Hypertrophied inferior transverse scapular ligament
- Scapulothoracic dyskinesia, shoulder girdle dysfunction
- Tension on the suprascapular nerve from lateralization during a supraspinatus and infraspinatus repair8 See the image below.
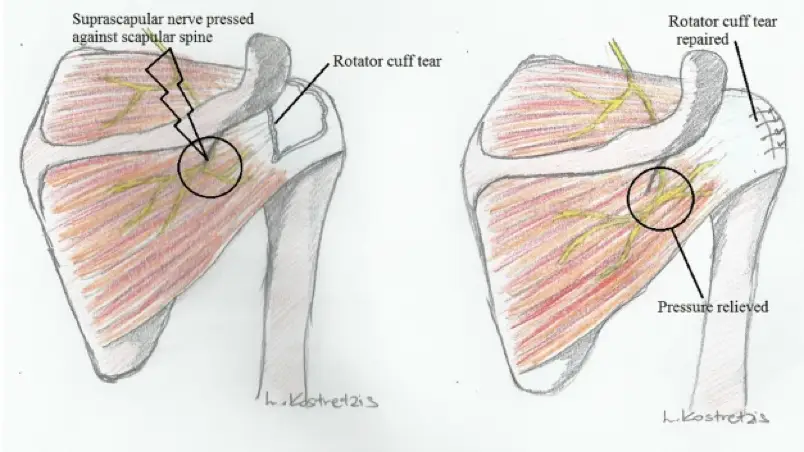
Overhead activities and sports, like volleyball, baseball, tennis, etc, also put stress on the suprascapular nerve through dynamic compression. In a study by Holzgraefe on elite volleyball athletes, they reported having a suprascapular neuropathy in as high as 33% of the athletes in their dominant arm/hand.9 Another study found an association between increased shoulder range of motion and isolated infraspinatus weakness.10 The proposed reason for the cause of the suprascapular neuropathy is that when the shoulder is in throwing motion it goes into extreme external rotation and abduction and causes the supraspinatus and infraspinatus muscles to impinge on the scapular spine, which compresses the motor branch to the infraspinatus.11, 12 Another proposed causation for the suprascapular neuropathy with overhead athletes is from damage to the axillary and suprascapular artery and therefore causing microemboli to the suprascapular nerve vasa nervorum.1, 13
Outside of compressive neuropathies, another condition that often affects the suprascapular nerve is Parsonage-Turner syndrome.
History and Examination
Patients with a suprascapular nerve will typically present with a dull, aching pain in the superior and posterolateral shoulder and often with radiating symptoms up to the neck or down the arm.1,2, 15 However if the problem is at the spinoglenoid notch, the patient may not complain of pain at all.2 If the patient is an overhead athlete, there should be a heightened level of suspicion for a suprascapular nerve issue.1,2 The patient may complain of a loss of function and weakness in the shoulder. Usually, a suprascapular neuropathy usually develops over time, but may also result from a traumatic event in upwards of 40% of patients.14
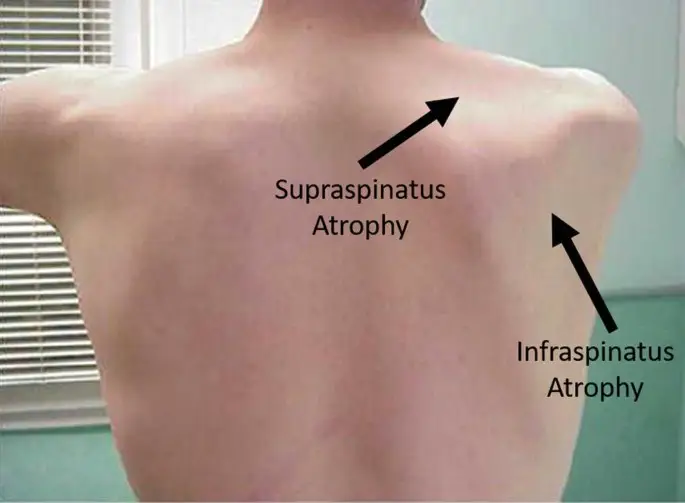
With multiple conditions that can present with similar symptoms, a thorough physical exam should be performed on bilateral shoulders as a comparison. The patient should be asked about and inspected for a previous shoulder surgery, any penetrating traumas, or fractures. The shoulder should be assessed for any atrophy in supraspinatus or infraspinatus (image above19), involve palpation of the AC joint and supraspinatus fossa for tenderness, weakness with shoulder abduction and external rotation, and any signs of instability to the shoulder joint. The neck may also produce similar symptoms, so a thorough neurological screen should also be performed.

Some additional special tests to assess for the suprascapular neuropathy include putting the shoulder into cross-body adduction and internal rotation and performing the suprascapular nerve stretch test. With the patient’s arm placed in cross-body adduction and internal rotation, the test would be considered positive when there is an exacerbation of their pain.15 The suprascapular nerve stretch test involves the clinician stands behind the patient, gently holds the head of the patient in lateral rotation away from the affected shoulder while retracting the affected shoulder with his other hand (image to the right). A positive test is when pain is reproduced or exacerbated in the posterior aspect of the shoulder.16
Diagnosis of a Suprascapular Nerve
The gold standard for diagnosing a suprascapular neuropathy is through electromyography and a nerve conduction study. In testing of patients with weakness, the accuracy of the EMG and NCS for suprascapular nerve pathology was as high as 91%.17 Findings positive for suprascapular pathology include fibrillation potentials and positive sharp waves, reduction in suprascapular nerve CMAP amplitude20, and increased latency. In the case of compression of the suprascapular nerve at the spinoglenoid notch, there may be a prolonged latency of the suprascapular nerve when recorded from the infraspinatus and/or fibrillation potentials or positive sharp waves only present in the infraspinatus and not the supraspinatus.
Magnetic resonance imaging of the shoulder is also helpful to assess the shoulder to evaluate for suprascapular nerve pathology by assessing for supraspinatus and infraspinatus atrophy. 18 It can also assess for soft tissue masses around the shoulder and labrum that could cause compression to the supraspinatus and for any rotator cuff pathologies.
Another way to help differentiate a suprascapular nerve neuropathy from other shoulder pathology can include an injection of anesthetic into the suprascapular and spinoglenoid notch and assess for pain relief in the shoulder and shoulder blade.1
Conclusion
Overall, suprascapular nerve pathology needs to be in the differential diagnosis of patients with shoulder pain and possible radiating symptoms, especially for individuals who are overhead athletes or if they present with pain in the superior and posterolateral shoulder and shoulder blade. In order to properly assess for a possible suprascapular neuropathy, the combination of a thorough physical assessment and neurological screening should be used along with electrodiagnostic (EMG and NCS) testing and MRI to confirm pathology and assess for causation.

Randall Hulet, PT, DPT, ECS
References:
- Kostretzis, L., Theodoroudis, I., Boutsiadis, A., Papadakis, N., & Papadopoulos, P. (2017). Suprascapular Nerve Pathology: A Review of the Literature. The open orthopaedics journal, 11, 140–153. https://doi.org/10.2174/1874325001711010140 (all images are included in this reference)
- Reece, C. L., Varacallo, M., & Susmarski, A. J. (2023). Suprascapular Nerve Injury. In StatPearls. StatPearls Publishing.
- Vorster W, Lange CP, Briët RJ, et al. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elbow Surg 2008; 17(3): 500-2. [http://dx.doi.org/10.1016/j.jse.2007.10.008]
- Bigliani LU, Dalsey RM, McCann PD, April EW. An anatomical study of the suprascapular nerve. Arthroscopy 1990; 6(4): 301-5. [http://dx.doi.org/10.1016/0749-8063(90)90060-Q] [PMID: 2264898] [20]
- Bayramoğlu A, Demiryürek D, Tüccar E, et al. Variations in anatomy at the suprascapular notch possibly causing suprascapular nerve entrapment: an anatomical study. Knee Surg Sports Traumatol Arthrosc 2003; 11(6): 393-8.
- Sjödén GO, Movin T, Güntner P, Ingelman-Sundberg H. Spinoglenoid bone cyst causing suprascapular nerve compression. J Shoulder Elbow Surg. 1996 Mar-Apr;5(2 Pt 1):147-9.
- Albritton MJ, Graham RD, Richards RS II, Basamania CJ. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elbow Surg 2003; 12(5): 497-500.
- Warner JP, Krushell RJ, Masquelet A, Gerber C. Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am 1992; 74(1): 36-45
- Holzgraefe M, Kukowski B, Eggert S. Prevalence of latent and manifest suprascapular neuropathy in high-performance volleyball players. Br J Sports Med 1994; 28(3): 177-9
- Witvrouw E, Cools A, Lysens R, et al. Suprascapular neuropathy in volleyball players. Br J Sports Med 2000; 34(3): 174-80. [http://dx.doi.org/10.1136/bjsm.34.3.174]
- Sandow MJ, Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg 1998; 7(5): 516-21. [http://dx.doi.org/10.1016/S1058-2746(98)90205-1]
- Ferretti A, Cerullo G, Russo G. Suprascapular neuropathy in volleyball players. J Bone Jt Surg – Ser A 1987; 69(2): 260-3.
- Ringel SP, Treihaft M, Carry M, Fisher R, Jacobs P. Suprascapular neuropathy in pitchers. Am J Sports Med 1990; 18(1): 80-6.
- Martin SD, Warren RF, Martin TL, Kennedy K, O’Brien SJ, Wickiewicz TL. Suprascapular neuropathy. Results of non-operative treatment. J Bone Joint Surg Am. 1997 Aug;79(8):1159-65.
- Plancher KD, Luke TA, Peterson RK, Yacoubian SV. Posterior shoulder pain: a dynamic study of the spinoglenoid ligament and treatment with arthroscopic release of the scapular tunnel. Arthroscopy. 2007 Sep;23(9):991-8.
- Lafosse L, Piper K, Lanz U. Arthroscopic suprascapular nerve release: indications and technique. J Shoulder Elbow Surg. 2011 Mar;20(2 Suppl):S9-13.
- Nardin RA, Rutkove SB, Raynor EM. Diagnostic accuracy of electrodiagnostic testing in the evaluation of weakness. Muscle Nerve 2002; 26(2): 201-5.
- Mellado JM, Calmet J, Olona M, et al. MR assessment of the repaired rotator cuff: prevalence, size, location, and clinical relevance of tendon rerupture. Eur Radiol 2006; 16(10): 2186-96.
- Plancher, K.D., Dotterweich, K.A., Commaroto, S.A., Wang, K., Briggs, K., Petterson, S.C. (2023). Endoscopic Suprascapular Nerve Decompression at the Spinoglenoid and Suprascapular Notches. In: Lui, T.H. (eds) Arthroscopy and Endoscopy of the Shoulder. Springer, Singapore. https://doi.org/10.1007/978-981-19-7884-5_59
- Kimura, J. (2013a). Mononeuropathies and Entrapment Syndromes. In Electrodiagnosis in diseases of nerve and muscle: Principles and practice (4th ed., pp. 761–761). essay, Oxford University Press.