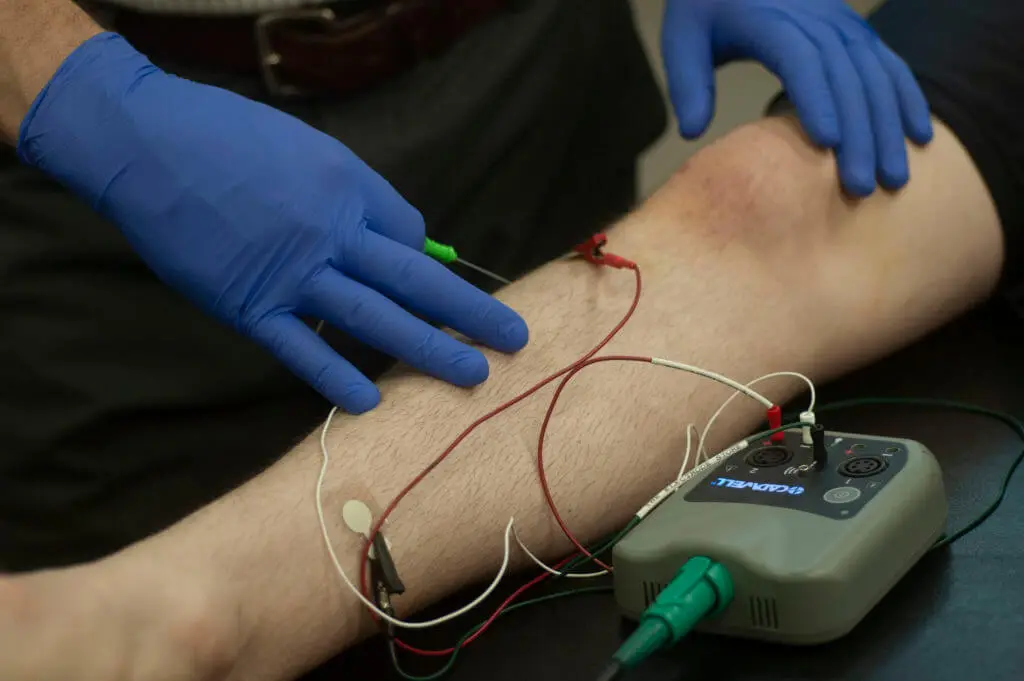
I have been practicing clinical electromyography (EMG) and nerve conduction studies (NCS) as a physical therapist for over 20 years and whenever I talk about it with other providers, their eyes begin to glaze over almost immediately. Their minds wander off to more pleasant experiences such as the beach, dinner and a movie or even getting their eyebrows threaded. I always think to myself, “If only they understood the great treasures that would be unfolded to them and their practice if they took a small amount of time and effort to understand even the basics of EMG/NCS and how it can enhance their practice.” You see, no other healthcare provider is better suited to perform EMG/NCS services on patients than physical therapists: we have a strong understanding of the neuromuscular systems, precise knowledge of anatomy and great patient bed-side manner. All three are crucial for obtaining good, reliable information and providing a positive experience for the patient. Additionally, studies have shown that physical therapists conform to the standards of practice for clinical EMG/NCS better than their physician counterparts1.
Physical therapists have been performing EMG/NCS for over 45 years and are even the authors of the official NIOSH manual published in 1990 by the federal government describing the standards for performing common nerve conduction studies2, distributed worldwide and referenced in many articles and books. The EMG/NCS test must be performed as an extension of the clinical exam. Findings of the EMG/NCS in isolation are not diagnostic, but, in combination with the clinical exam and other diagnostic testing, such as imaging and lab work, it is a useful tool assisting in the formation of a diagnosis. Additionally, the APTA has specified in the 2001 publication of Guide to Physical Therapist Practice3 that physical therapists perform electroneuromyography (EMG/NCS) and use electroneuromyographs to assess electrophysiological integrity of motor function, muscle performance, peripheral nerve integrity, etc. as part of the tests and measures. But what does that matter to you? When you see a report, you see nonsensical verbiage, meaningless numbers and graphs. What does it all mean? In this two part blog, I will attempt to eradicate the mystery and arcaneness of the EMG/NCS report. Part one of this blog will discuss basics of nerve and muscle disease, principles of the NCS and how to read the data in a report. Part two, which will appear at a later date, will cover principles of needle EMG, specific diseases and injuries and how EMG/NCS findings relate to outcomes for certain injuries and surgeries of the upper extremities.
Why is it important for healthcare providers to understand the EMG/NCS report? Some of the answers to this question include: 1. Poor correlation of clinical examination findings to actual disease for some disorders such as carpal tunnel syndrome4, 5, 2. The electrodiagnostic (EDX) testing provides insight into the health and function of the nerve’s myelin, axons, neuromuscular junction, and muscular disease and possible outcomes of treatment, 3. EDX testing can provide focus and clarification of known issues and possibly uncover previously unknown issues inhibiting the patient’s ability to improve with normally effective treatments.
Understanding the Neurophysiology
A normal healthy peripheral nerve, such as the median nerve, is made up of thousands of individual nerve fibers coated in myelin. The myelin cells, by coating the axons, are responsible for the conduction speed of the electrical signal along the nerve axons (salutatory conduction). Each nerve fiber is encased in an endoneurial sheath which provides the basic supporting structure. Many of these nerve fibers are then grouped together by the perineurium forming a fascicle. Multiple fascicles are then tightly bound together by the epineurium forming the nerve proper. An injury may affect individual fibers, one or more fascicles or the entire nerve. Seddon6 classified nerve injuries into three categories: neurapraxia, axonotmesis and neurotmesis. Neurapraxia is a signal conduction loss without structural damage to the axon but with damage to the myelin, resulting in a slowed signal conductance across the site of injury (such as in carpal tunnel syndrome). Once the cause of the injury is removed, recovery occurs within days or weeks and remyelination ensues if demyelination occurred. Axonotmesis involves the maintenance of collagenous supporting structures, but loss of continuity of the axons with accompanying Wallerian degeneration of the distal segment. In some instances, partial injury of select fascicles may occur resulting in an incomplete injury to the nerve and non-classical demonstration of symptoms. Recovery is slow even under optimal conditions, at a rate of 1 to 3 mm/day and may take months or years to fully resolve. Neurotmesis involves the complete separation of the entire nerve and its supporting structures, such as when cut by a knife. This results in a total loss of signal conduction across the site of injury. Recovery usually requires surgical intervention and can result in a poorly organized or incomplete repair.
Understanding a Waveform
Understanding a waveform and related terminology are crucial to understanding an EMG/NCS report. When a NCS is performed, the recording electrodes are placed either directly over the nerve, in the case of sensory testing or over a muscle corresponding to the nerve being evaluated, in the case of motor testing. The nerve is then stimulated at a specific distance from the recording electrodes. Typically for motor nerves this distance is 8 cm and for sensory nerves 14 cm. This most distal segment of evaluation is termed the “distal or terminal latency.” Sensory studies can be performed either in an orthodromic fashion (in the same direction that the nerve signal normally travels which is distal towards proximal) or antidromically (proximal towards distal). Either direction is acceptable and should be referenced on the report. The recorded signal is called a sensory nerve action potential (SNAP). Motor studies can only be performed in an orthodromic fashion because the neuromuscular junction (NMJ) is unidirectional. The resulting signal is a compound motor action potential (CMAP). By convention, an upward deflection of the waveform is called a negative deflection and conversely, a downward deflection of the curve is termed a positive deflection. The recorded CMAPs and SNAPs may look similar but are distinct and referenced differently.
Traditionally, sensory distal latencies, recorded in milliseconds (ms) have been measured from the point of stimulation to the peak (see Figure 1), although it has become more and more common to see them referenced to the initial negative deflection. The sensory distal latency measured to the peak is a representation of the mode speed of the fibers (most fibers with the same speed). For sensory waveforms whose distal latency is measured to the peak, the amplitudes are measured in microvolts (μV) from the negative peak to the positive peak. The negative area under the curve in conjunction with the amplitude is a representation of the number of axons carrying a nerve signal.
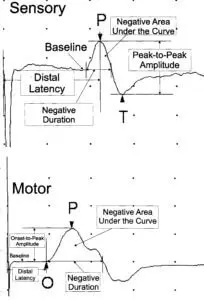
Motor waveform distal latencies are measured in ms from the point of stimulation to the initial negative deflection of the curve, representing the very fastest motor fibers in the nerve (see Figure 1). Motor nerve amplitudes are measured in millivolts (mV) from the baseline to the negative peak of the curve. Similarly to the sensory waveform, the negative area under the curve in conjunction with the amplitude is a representation of the number of motor axons carrying a nerve signal. The negative duration for both motor and sensory nerves is related to the statistical range of distal latencies of all the nerve fibers. A shorter negative duration signifies that all the nerve fibers are carrying signals at similar speeds and function.
Nerve Conductions
Nerve conductions are another valuable part of the NCS test and are used to evaluate segments of nerves, such as the ulnar nerve across the elbow or the median nerve across the forearm. The nerve conduction velocity is obtained by calculating the difference in latencies between two stimulation points (see Figure 2). If the distal latency is 3.3 ms and the elbow latency is 7.7 ms then the delta latency is 4.4 ms. The distance between these two stimulation points (wrist to elbow) is measured in millimeters (230 mm) and is divided by the delta latency (4.4 ms), resulting in the formula of 230 mm/4.4 ms = 52 m/s.
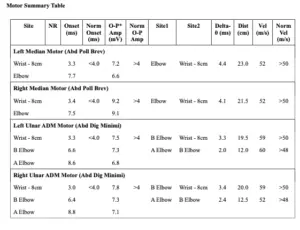
NCS findings are a good way to evaluate nerves over segments and are best applied to short segments; however, segments shorter than 10 cm should be avoided if possible. Segments shorter than 10 cm can accentuate small technical errors and may inadvertently provide false positives or false negatives. Nerve conduction velocities across long segments may hide small or mildly affected points of injury since the faster portions of that segment may average out the slower points to a velocity that is within normal limits. To assist with identifying milder injuries, the examiner may perform “inching studies” wherein the longer segments are broken into very small segments (e.g., a 10 cm segment is broken down into five 2 cm segments) to help isolate the affected area. When slowed segments affecting multiple nerves are noted, findings may suggest a systemic disease process. Nerve conduction testing of at least three extremities will help to clarify those findings. In general, when referring to the upper extremities, motor nerve conductions should be greater than 50 m/s and sensory nerve conductions should be at least 39 m/s. Some providers allow for slightly slower nerve conductions across the elbow due to normal wear and tear of the superficially positioned ulnar nerve.
Conclusions
In part two, which will appear in subsequent blog, we will discuss the needle EMG, pertinent diseases and injuries, and pull it all together to make sense of it all. Whether your patient has carpal tunnel syndrome, cubital tunnel syndrome or more complex problems such as a brachial plexus injury, understanding the EMG/NCS report will help guide appropriate therapies. Studies have related EDX findings to outcomes for several different diseases and their treatments. Appropriately interpreting the findings of the EDX test can help the patient and provider to set reasonable goals, apply appropriate treatments and attain better outcomes, ultimately improving the patient’s mobility and long term function.
- Armantrout EA, Hummel-Berry K, Underwood F, Nelson C. Physical therapist compliance with electromyography guidelines. JNPT. 2008;32:177-185.
- Performing Motor and Sensory Neural Conduction Studies in Adult Humans. NIOSH Manual #90-113, 1990.
- Guide to Physical Therapist Practice. Second Edition. American Physical Therapy Association Phys Ther. 2001 Jan;81(1):9-746.
- El Miedany Y, Ashour S, Youssef S, Mehanna A, Meky FA. Clinical diagnosis of carpal tunnel syndrome: old tests-new concepts. Joint Bone Spine. 2008 Jul;75(4):451-7.
- MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004 Apr-Jun;17(2):309-19.
- Seddon HJ. Three types of nerve injury. Brain. 1943;66:237-288.