Traumatic Neuroma- nerve damages from outside the common compression neuropathy.
Introduction
We encounter various neuropathic symptoms and pain every day. Patient reports of neuropathic pain can differ in descriptions, characteristics, and patterns. It is crucial for healthcare providers, especially those working in diagnostics, to understand which pathological presentations necessitate more direct interventions, such as surgery and injections, and which may benefit from indirect methods like physical therapy, desensitization, and medications. This knowledge is essential for informed and effective healthcare decision-making.
In the context of neuralgia, it encompasses a wide range of symptoms and pain mediated by various nerve fibers or processes.
Certain conditions in centralized neuropathy are acquired and can result from inappropriate treatments for nerve damage. 1, 2 Unlike peripheral-mediated neuralgia, central neuropathy cannot be relieved through direct treatment to the damaged nerve. 2 There have been reported cases indicating that certain central neuropathies are linked to nerve damage and unsuccessful treatments. Recognition of the types of nerve damage and expedited implementation of appropriate treatments for damaged nerves may contribute to the prevention of central neuropathies in some instances.3,4
Pathomechanisms
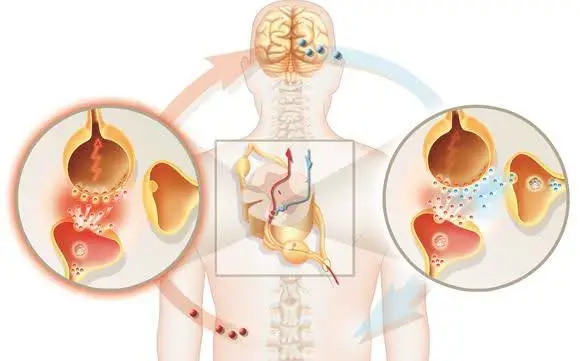
Recent research findings indicate that the entire pathway from the target organ or sensory receptor to the brain cortex plays a pivotal role in nerve regeneration and neuralgia.1 In the context of motor nerves, this pathway encompasses the motor cortex, alpha motor neuron, neuromuscular junction, and muscle. For sensory nerves, the pathway involves the sensory receptor, dorsal root ganglion, and second-order sensory neuron. Understanding and considering the integrity and function of each component along these pathways are crucial in comprehending nerve regeneration processes and addressing issues related to neuralgia.
Central neuropathic pain, including conditions like hyperalgesia and phantom pain, can arise due to collateral sprouting and cortical remodeling, respectively.1
Central-mediated pain, such as poststroke pain or phantom pain, underscores the significance and complexity of the central nervous system’s role in persistent pain. If the central nervous system and cortical remodeling are indeed linked to pain, the available treatment options remain unclear.5
On the contrary, compression neuropathy and traumatic neuroma suggest the need for directive interventions.
Moreover, in cases where compression neuropathy or neuroma is treated improperly, they may lead to centrally mediated neuralgia, such as hyperalgesia and phantom pain, which can be preventable.
Neuroma-in-continuity is a subtype of neuroma that remains connected within the nerve’s continuity. It is reported to develop from Seddon’s classification 2 axonotmesis or Sunderland classification 2-4. This type of neuroma can arise not only from high-energy injuries like avulsion, transection, or stretch but also from low-energy injuries such as entrapment, compartment pressure, injection injury, or contusion.6,7 In such cases, the formation of neuroma-in-continuity may occur beyond the typical sites associated with common compression neuropathy. When neuroma-in-continuity forms, it has the potential to initiate Wallerian degeneration through endoneurial damage.8,9

Diagnostics
The localization of the compression site or neuroma formation site is crucial in determining the appropriate treatment option. A thorough physical examination, comprehensive history-taking, and the application of diagnostic tools such as NCS/EMG should suffice to identify the lesion.
Conclusions
There is no standardized protocol for neurological examination in cases of injury outside the common compression neuropathy area. However, given the potential severe consequences of misdiagnosis or mistreatment of such non-common neuropathic pain, it is crucial to conduct a thorough examination with care. Recommending follow-up exams or utilizing morphological nerve testing tools, such as US or MRI, to visualize and assess nerve damage as needed is advisable.

References
- Finnerup et al., (2021), Neuropathic pain: from mechanisms to treatment. Physiol Rev 101: 259–301, https://doi.org/10.1152/physrev.00045.2019
- Dorsi MJ, Chen L, Murinson BB, Pogatzki-Zahn EM, Meyer RA, Belzberg AJ. (2008) The tibial neuroma transposition (TNT) model of neuroma pain and hyperalgesia. Pain. 134:320-334
- Abdo H, Calvo-Enrique L, Lopez JM, et al. (2019) Specialized cutaneous Schwann cells initiate pain sensation. Science. 365:695-699.
- Doan RA, Monk KR. (2019) Glia in the skin activate pain responses. Science. 2019;365: 641-642.
- E.J.R. Hill et al. (2023) What is Operative? Conceptualizing Neuralgia: Neuroma, Compression Neuropathy, Painful Hyperalgesia, and Phantom Nerve Pain. Journal of Hand Surgery Global Online 5 126-132.
- Gentili F, Hudson AR, Midha R. (1996) Peripheral nerve injuries: types, causes, and grading. In: Wilkins RH, Rengachary SS, eds. Neurosurgery. New York, NY: McGrew-Hill; 1996:3105–3114.
- Speed JS, Knight RA. (1956) Peripheral nerve injuries. Campbell’s Operative Orthopedics. St. Louis, MO: C.V. Mosby; 1956:947–1014.
- Al-Majed AA, Brushart TM, Gordon T. (2000) Electrical stimulation accelerates and increases expression of BDNF and trkB mRNA in regenerating rat femoral motoneurons. Eur J Neurosci 2000;12(12):4381–4390.
- Siironen J, Sandberg M, Vuorinen V, Röyttä M. (1992) Expression of type I and III collagens and fibronectin after transection of rat sciatic nerve. Reinnervation compared with denervation. Lab Invest 1992;67(1):80–87.


