A patient comes to see you with wrist drop. As you are an astute clinician you infer that the patient has a radial nerve injury, but how do you know where the likely cause of injury is? A thoughtful and thorough clinical exam should shed some light on the situation.

Wrist Drop. Image source: Flickr Commons
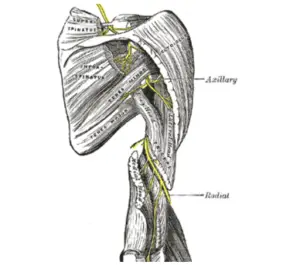
Radial nerve injuries occur most frequently after fracturing the middle third of the humerus.1 However, there are many sites of possible compromise leading to wrist drop including at the axilla, at the spiral groove, or at the arcade of Frohse. Let us take a look at each one of these sites and see what clinical findings we might see.

War correspondent Ear Crotchett on crutches. Image source: Flickr Commons
Axilla
A compromise in the axilla is commonly caused by riding high with axillary crutches and is known as crutch neuropathy.2 A radial nerve injury this proximal to the brachial plexus will cause many clinical findings. The patient may have weakness with manual muscle testing of elbow extension, wrist extension, and finger extension. The patient will also complain of paresthesia in a superficial radial sensory nerve distribution including the dorsum of the hand and possibly along the posterior forearm, as the posterior cutaneous nerve to the forearm may also be affected.
The radial or spiral groove of the humerus. Image source: Wikimedia Commons.
Spinal Groove of the Humerus
A compromise of the radial nerve in the spiral groove (radial groove) is commonly known as “Saturday night palsy” as it normally occurs when one falls into a deep sleep after a night of drinking.2 Similar to compression at the axilla, the patient will have a weakness with elbow extension, as well as weakness of the wrist extensor and finger extensor muscles. However, there will be nerve preservation to the medial head of the triceps and anconeus muscles as these nerve fibers branch off to innervate these muscles proximal to the spiral groove. Thus, the patient should be able to extend their elbow much better than if the radial nerve compromise were more proximal. The patient will also complain of paresthesia in a superficial radial sensory nerve distribution including the dorsum of the hand but likely not along the posterior forearm, as the posterior cutaneous nerve to the forearm branches off proximal to the spiral groove as well.

Lateral elbow. Image source: Wikimedia Commons.
Arcade of Frohse
A compromise of the radial nerve as it passes through the two layers of the supinator muscle in the arcade of Frohse is called supinator syndrome or posterior interosseous nerve syndrome.2 The patient will have normal elbow extension, normal supination, and normal sensation as only the posterior interosseous innervated muscles will be affected due to the fact that the superficial radial sensory nerve branches off proximal to the supinator muscle. Thus, the patient will have a weakness with wrist extension and finger extension only.
These are not the only possible sites of radial nerve compromise but are the most common which will lead to wrist drop. One could also have an isolated superficial radial sensory nerve compromise that would lead only to sensory findings without any motor involvement. If the patient is in a car accident, has been shot or stabbed, had an injection, or even had some type of crush injury the possible site of the lesion could be anywhere along the length of the arm.
A thorough clinical exam can lead to a proper diagnosis and electrodiagnostic testing can help aid in distinguishing the exact injury location and the degree of damage.3 If you or your patients are in need of expert evaluation, we here at EMG Solutions can help.

- Stern, M., MD, & Gellman, H., MD. (2020, February 24). Radial Nerve Entrapment. Retrieved March 17, 2021, from https://emedicine.medscape.com/article/1244110-overview#a7.
- Leis, A. A., & Trapani, V. C. (2000). Atlas of Electromyography. Oxford, NY: Oxford University Press.
- Bumasirevic, M., Palibrik, T., Lesic, A., & Atkinson, H. (August 2016). Radial Nerve Palsy. Effort Open Reviews, 1, 286-294. doi:10.1302/2058-5241.1.000028. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367587/.


