Many patients are told, “You have sciatica.” You have lumbago, a lumbar radiculopathy, you have a pinched nerve at your lower back, a slipped disc, neuralgia, spondylosis… the list seems to go on and on. These injury designations are often used interchangeably and seem to be the same thing but at the same time are incredibly different. While each of these is usually associated with lower back and/or hip pain that may or may not run down the leg, they are hinting at a possible nerve compression. A true nerve compromise whether it is at your back or along the length of the sciatic nerve will present very differently depending upon the location of the problem.
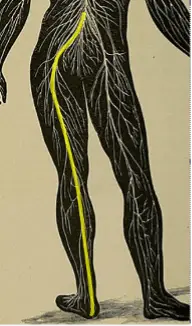
According to the Mayo Clinic, “Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. Typically, sciatica affects only one side of your body.”1 The sciatic nerve is the largest nerve in the body that stems from the L4 through S3 nerve roots.2 After the anterior rami leave the nerve root levels, they coalesce into one nerve and descend through the greater sciatic foramen passing underneath the piriformis muscle. As the nerve continues down the leg it branches out into the tibial and fibular nerves just before the back of the knee. The tibial nerve innervates the more posterior leg musculature down into the foot, while the fibular nerve innervates the anterior and lateral lower leg musculature. This means there are a lot of areas of potential compromise.
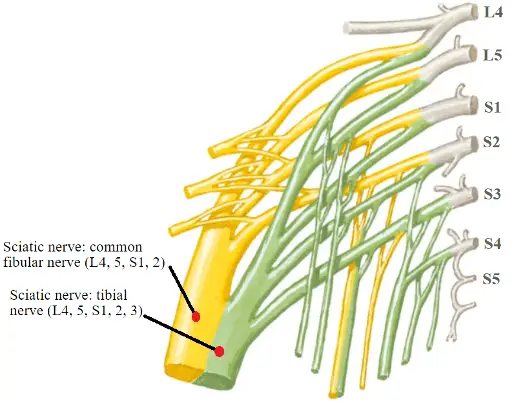
A true sciatic nerve compromise typically occurs anywhere after the sciatic nerve first arises from the lumbosacral plexus to just proximal to the back of the knee where the fibular and tibial nerves branch out. Tumors, trauma, traction, radiation therapy, compression injuries, muscular entrapment, and intramuscular injections can cause sciatic nerve issues, just to name a few.3 The location of the exact area of compromise will affect what kind of symptoms and deficits will make up each patient’s complaints. However, no matter where the sciatic nerve is injured similar findings will be seen in the lower leg.
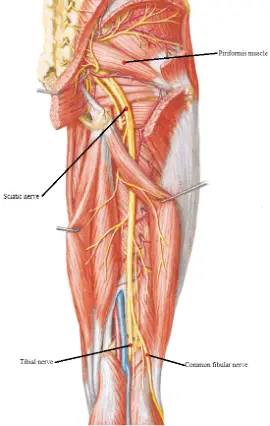
An injury to the sciatic nerve in the upper leg will affect the tibial and fibular nerve branches which are oriented more distally. For example, if the compromise is closer to the posterior knee, the patient will have preservation of the hamstring musculature, but will have foot drop, ankle plantar flexion weakness, as well as paresthesia of the entire foot and lateral lower leg. While a nerve injury more proximally located around the piriformis muscle will have all the same abnormal previous findings, but with the added weakness of the hamstring muscles.
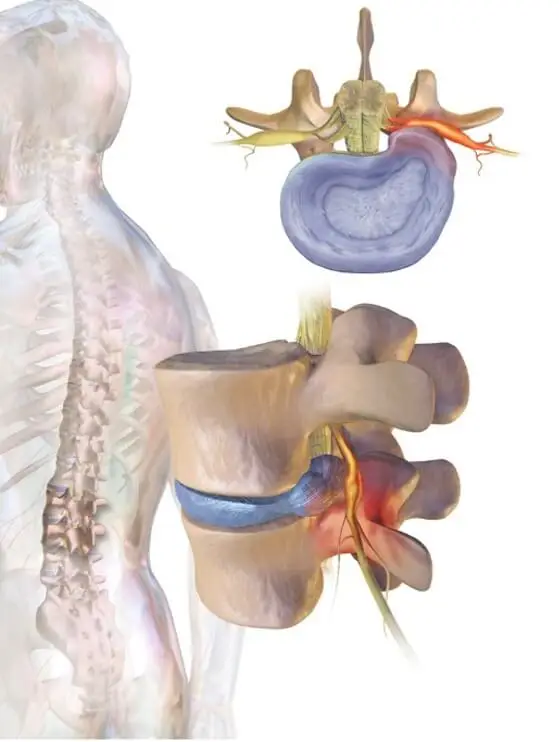
Now if the problem is in fact a pinched nerve at the L5 and S1 nerve root levels at the lower back and not the sciatic nerve, clinically the patient will present very similarly. Most patient complaints will include leg weakness, numbness and tingling of the lower leg, and radiating symptoms. Yet, a pinched nerve at the lower back and a sciatic nerve compromise should be treated very differently. So how can one tease out the difference between a pinched nerve at the lower back versus a sciatic nerve compromise?
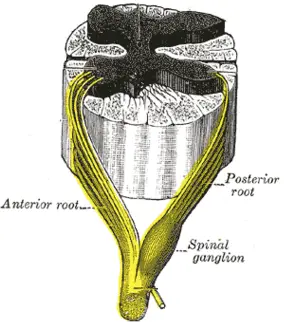
This is where further testing is needed, imaging alongside nerve conduction studies (NCS) combined with electromyography (EMG) can help locate a nerve compromise more definitively. Making the distinction between these two specific ailments revolves around the fact that the sensory nerve cell bodies lie outside of the spine in the dorsal root ganglion (or spinal ganglion). This means that if the problem is a compressed nerve root (at the spine) the sensory nerve cell body and its connection to the nerve fibers will be preserved, and the sural and superficial fibular sensory nerve studies will be normal with NCS testing. However, if the problem is the sciatic nerve, one or both of these sensory nerves will also be abnormal.
A good clinical history and physical exam alongside other diagnostic tests, such as EMG/NCS can help to rule in or rule out a nerve compromise. If you, a friend, a family member, or your patients are in need of expert evaluation, we here at EMG Solutions are happy to help.
- Mayo Clinic Staff. (2020, August 1). Sciatica. Mayo Clinic. Retrieved April 6, 2022, from https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435
- Giuffre BA, Jeanmonod R. Anatomy, Sciatic Nerve. [Updated 2021 Jul 29]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482431/
- Leis, A. A., & Trapani, V. C. (2000). Atlas of electromyography. Oxford: Oxford University Press.




