A patient comes to see you with numbness and tingling of the right ring and little fingers. As you are an astute clinician you infer that the patient either has an ulnar nerve injury or a possible C8 cervical radiculopathy, but how do you know exactly where the likely cause of injury is? A careful and considerate clinical exam should lead you in the right direction.
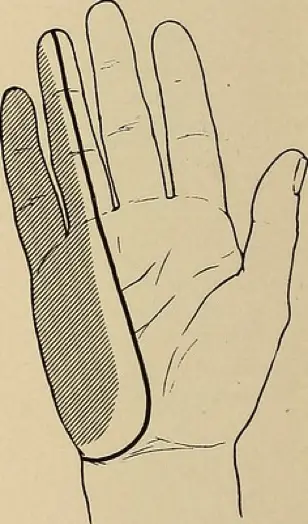
Paresthesia of the medial hand. Image source: Flickr Commons
First and foremost, it can be challenging to distinguish between a cervical radiculopathy versus ulnar neuropathy with clinical exam testing alone. However, with an experienced electromyographer simply looking at the ulnar sensory nerve, an ulnar neuropathy can be ruled in or out in a matter of a few minutes. If the ulnar sensory nerve is abnormal the problem is a peripheral nerve compromise whereas if the ulnar sensory nerve is present and within normal limits a C8 cervical radiculopathy becomes more likely. For our sake let’s imagine the problem is in fact an ulnar neuropathy, how can we distinguish where the ulnar nerve compromise is located?
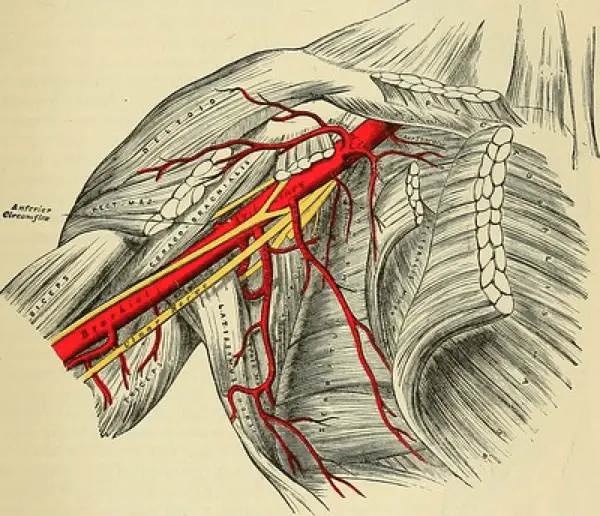
Ulnar nerve at the axilla. Image source: Flickr Commons
Axilla
A compromise in the axilla can occur due to some type of traumatic event such as a car accident, gun shot, or stabbing injury. An ulnar nerve injury this proximal to the brachial plexus will cause many clinical findings. The patient will have weakness with manual muscle testing of ulnar wrist deviation, wrist flexion, finger flexion of digits 4 and 5, as well as finger abduction and adduction. The patient will also complain of paresthesia of the medial aspect of the hand including the little and medial half of the ring fingers.
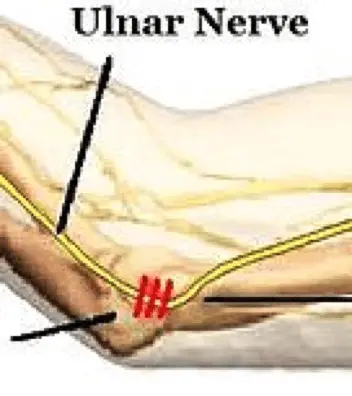
The ulnar nerve at the elbow. Image source: Wikimedia Commons.
Medial Elbow
A compromise of the ulnar nerve at the elbow is a common area of injury and compression.1 There are two specific sites at the elbow where the ulnar nerve is often compressed. The retrocondylar groove or area just proximal to the medial epicondyle, as well as the cubital tunnel which is at and just distal to the medial epicondyle.3 There is a difference in the way the ulnar nerve is treated surgically depending upon the area of entrapment.3 This can be more localized with NCV testing of the ulnar nerve.
An ulnar nerve compromise at the elbow, regardless of which area is the site of entrapment will present the same. The patient will complain of numbness and/or tingling over the medial aspect of the hand including the little and medial half of the ring fingers. They may also complain of grip weakness and difficulty spreading their fingers apart. You may notice muscular atrophy of the first dorsal interosseous or the adductor digiti minimi as these muscles are the most easily observed. Patient’s typically have normal strength with ulnar deviation of the wrist.
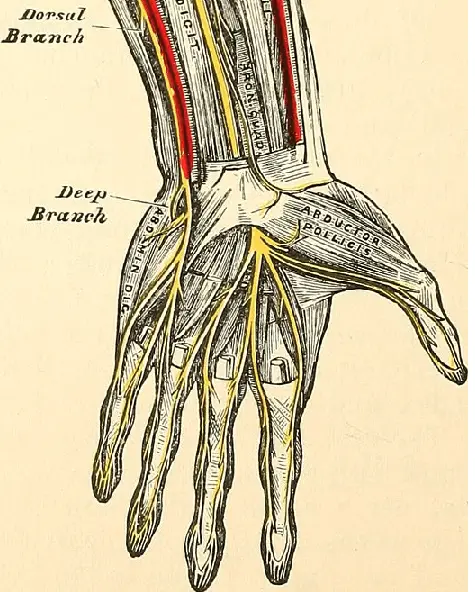
Ulnar nerve at the wrist. Image source: Flickr Commons.
Wrist – Guyon’s Canal
Depending upon where the site of injury is located at the wrist or hand will determine how a patient will describe their symptoms. There are three different zones where the ulnar nerve can be compromised.
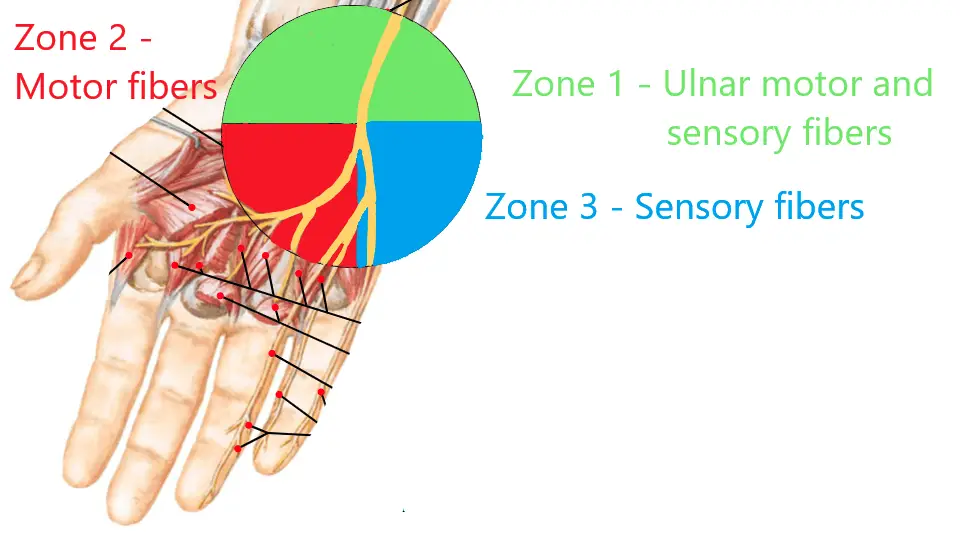
Ulnar nerve at the wrist. Image source: Netter’s Atlas
A patient with a compromise of the ulnar nerve in Zone 1 will present with both sensory and motor nerve abnormalities with NCV testing. They will likely complain of grip weakness since the interossei, lumbricals, and hypothenar muscles will all be affected.3 They will also complain of numbness and/or tingling in the ring and little fingers.
A patient with a compromise of the deep ulnar motor branch in Zone 2 will complain of only hand and grip weakness because this is a purely motor deficit causing weakness which will only affect the interossei and lumbricals but spare the hypothenar muscles.3 The ulnar sensory nerve will be present within normal limits.
A compromise in the proximal Zone 3 will cause the patient to have paresthesia of the ring and little fingers due to sensory nerve deficits as well as difficulty abducting the little finger due to the motor nerve deficits to the abductor digiti minimi muscle. There will be sparing of the deep ulnar motor innervated interossei and lumbricals.3 Lastly, a more distal Zone 3 compromise will cause purely sensory abnormalities and spare all intrinsic ulnar innervated hand musculature.3 Thus, complaints will be purely paresthesia without any weakness.
Depending upon the mechanism of injury other possible areas can be cause for concern. These areas include the ulnar nerve in the forearm and a medial cord compromise of the brachial plexus. A thorough clinical exam can lead to a proper diagnosis and electrodiagnostic testing can help aide in distinguishing the exact injury location and the degree of damage.3 If you or your patients are in need of expert evaluation, we here at EMG Solutions can help.

- Charles F Guardia, I. (2021, April 02). Ulnar neuropathy. Retrieved April 08, 2021, from https://emedicine.medscape.com/article/1141515-overview#a4
- Dy, C., & Mackinnon, S. (2016, April 14). Ulnar neuropathy: Evaluation and management. Retrieved April 06, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4896870/
- Leis, A. A., & Trapani, V. C. (2000). Atlas of electromyography. Oxford: Oxford University Press.


