Several weeks ago I published a blog describing the kinds of neurologic disorders revealed by electromyography and nerve conduction studies (EMG/NCS) in patients who are suspected of carpal tunnel syndrome (CTS) on clinical grounds. In most of these patients, EMG/NCS serves to confirm the presence of median nerve pathology and to describe how severe it is, but other disorders like radiculopathy and ulnar nerve compromises can also be found masquerading as carpal tunnel syndrome. A third possibility is that the test may yield normal results. Indeed, of the 338 patient records I examined, 14% of those referred with suspicion of CTS had no evidence of nerve damage found with electrodiagnostic testing.
So what is going on with these patients? This is a big question, but in this post, I hope to shed a little light as we explore a few of the possible causes for carpal tunnel-esque symptoms (pain, numbness, and tingling in the hands) which lie outside the realm of peripheral nerve dysfunction.
Where do Symptoms Come from Anyway?
In the first place, it is important to understand that all the things we feel—touch, pain, temperature, and even the “pins and needles” sensation of paresthesia—are products of our own brain interpreting the stimuli it receives.
When the nerves and the brain are working properly, the things we feel make sense: a fluffy cat feels like a fluffy cat and cold steel feels like cold steel. When peripheral nerves are damaged, however, they send confusing signals to the brain, and the brain in turn produces abnormal feelings like numbness and tingling.
But our brains can even create sensations without any peripheral nerve signals to cue them. The most classic example is phantom limb pain, where a person feels genuine discomfort in a hand or foot that no longer exists!
Similarly, when I was a boy, I would sometimes jokingly throw a punch past my younger brother’s shoulder, and when he would grab his arm and say, “That hurt!” I would argue back that “I didn’t even touch you!” As a medical professional I now understand that we were both right. My punch really didn’t make contact, but the mere sight of it was enough for his brain to generate the pain which seemed like an appropriate response to the anticipated hit.
Keep this in mind as we discuss some sources of hand symptoms which are not nerve related. Pain and other symptoms are always very real to the person experiencing them, but because they rely on the brain’s interpretation (and sometimes misinterpretation) of stimuli, they do not always line up well with their own causes.
1. Carpal Tunnel Syndrome
Before diving into other symptom causes, let me be the first to acknowledge that normal EMG findings do not necessarily mean that a person does not have carpal tunnel syndrome.
By definition, syndromes are conditions with multiple signs and symptoms which “run together” (the original Greek meaning of the word) to create a distinct pattern.
Median nerve dysfunction at the wrist, as measured by EMG/NCS, is one of the signs that contribute to CTS, but if other clinical signs paint a very clear picture, carpal tunnel syndrome can be diagnosed even with normal test results.
Indeed, some studies have shown that the majority of patients with a clear clinical diagnosis of CTS respond favorably to surgical intervention. That being said, surgical success rates are higher in those with electrodiagnostically established CTS. Thus, although normal EMG/NCS results do not absolutely preclude a carpal tunnel syndrome diagnosis, they do cast some doubt, and many physicians opt for conservative treatment strategies when EMG/NCS evidence is lacking.
2. Central Nervous System Disorders
Since sensations essentially come from the brain, pathology in the brain often creates abnormal sensations in the body.
For example, a stroke affecting the right postcentral gyrus (a part of the brain that receives sensory information) may leave a person unable to feel his or her left hand.
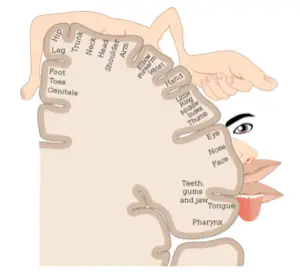
Figure 1: Areas of the postcentral gyrus responsible for sensation of various body parts. Image from: Wikimedia Commons.
Multiple sclerosis also often causes symptoms in the extremities, but because it is a central nervous system (brain and spinal cord) disorder it typically will not be detected by electrodiagnostic tests (which primarily evaluate peripheral nervous systems).
Disorders like these are uncommon, but if they exist in a patient’s history, they may help to explain why EMG/NCS tests come back normal.
3. Nutritional Deficiencies
Nerve signals (called “action potentials”) are generated within neurons through a complex series of chemical reactions. If there is not a proper balance of these chemicals in the body, then the nerves may not conduct properly even though they are structurally intact.
Important vitamins and minerals for nerve conduction include Potassium and the B vitamins. Too little or too much of these substances can cause an otherwise normal nerve to behave irregularly, resulting in changes to sensation.
Although nutritional deficiencies often do not damage nerves in the early stages, if the problem goes untreated for too long, widespread nerve damage (called neuropathy) can occur. It is worthwhile to discover and address any nutritional problems quickly.
4. Medication Side-Effects
The chemical reactions in and around nerves can also be affected by medications. Numbness and tingling can be a side-effect of many drugs, and although some medicines can be neurotoxic, others can cause these symptoms without damaging the nerves.
If the symptoms arise around the same time that a medication is introduced or discontinued or when the dosage changes, it may be worth considering a relationship between the two events.
5. Myofascial trigger points
“Trigger points” are tender, irritable parts of a muscle which often cause referred pain into other areas of the body. For example, trigger points in the shoulder can often refer pain down the arm to the hand.
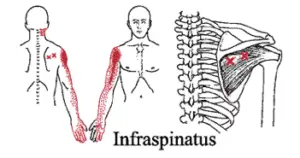
Figure 2: Trigger points in the infraspinatus muscle (marked “X” around the shoulder blade) can cause referred pain in the shoulder arm, and hand. Image from: Cascade Wellness Clinic.
The origins of referred pain are not fully understood, but one common theory is that nerve signals from one part of the body may cause the neurons of other body parts to activate if the two neurons are close to each other in the spinal cord.
In addition to pain, trigger points can sometimes result in abnormal sensations as well. There is limited research into trigger point treatments, but some case studies report significant improvements in upper extremity numbness and tingling following trigger point therapies.
If a patient with normal EMG/NCS results has pain in the neck, shoulder, or arm in addition to his or her hand symptoms it may be worthwhile to palpate the muscles in these areas and see if the hand symptoms can be reproduced by pressing on a trigger point elsewhere.
6. Central Hypersensitivity
As I mentioned at the start of this article, the sensations we feel rely both on the nerve signals that our bodies send to the brain and on how the brain interprets those signals.
Sometimes after an injury the central nervous system (brain and spinal cord) will attempt to protect the injured area by effectively going on “high alert.” It prioritizes any nerve signal that seems like it could be a threat and produces a large amount of pain or other symptoms to encourage us to be more careful while we’re injured.
The problem is that sometimes the high alert doesn’t end even after the initial injury heals. Sometimes the hypersensitivity even gets worse and starts to spread to other areas of the body.
The most severe cases can develop into a condition called complex regional pain syndrome (CRPS, also previously known as reflex sympathetic dystrophy or RSD), where even the lightest touch can cause excruciating pain, but even common disorders like osteoarthritis can result in hypersensitivity which mimics the pain, numbness and tingling normally associated with nerve disorders.
If a patient describes hand pain and sensory changes that began after a traumatic injury like a wrist fracture, but EMG/NCS test results are normal, then they may benefit from the care of a healthcare professional experienced in managing chronic pain conditions.
Summary
The conditions I have discussed here certainly do not constitute an exhaustive list. The human body is complex and each individual is unique, so a simple symptom like hand pain could have a multitude of possible causes.
If a patient’s history and clinical examination seem consistent with a peripheral nerve disorder like carpal tunnel syndrome then electrodiagnostic studies can help to confirm and/or clarify that suspicion. A negative test result may be just as helpful, however, as it invites further exploration to find other possible symptom explanations.
In my own practice I often tell my patients “I don’t wish nerve damage on anyone.” EMG/NCS tests can be an extremely powerful tool to identify nerve compromises, and I am always thrilled to discover disorders which will solve the mystery of a patient’s pain and lead to appropriate treatment and relief. On the other hand, I am equally happy to find normal results, because they can point a patient toward a medication change, dietary adjustment, myofascial release, or other therapy that will be equally effective.


